CNS Depression Risk Calculator
Risk Assessment Tool
This tool helps you understand the risks of combining valerian root with other substances that depress the central nervous system. Based on the article, mixing valerian with other sedatives can lead to dangerous additive effects.
How This Works
Based on the article, combining valerian with other CNS depressants creates additive effects that can lead to dangerous drowsiness, slowed breathing, or even loss of consciousness. This calculator identifies combinations that pose significant risk based on information from the NIH, Mayo Clinic, and WebMD.
Select your situation and click "Assess Risk" to see results.
Many people turn to valerian root as a natural way to improve sleep. It’s been used for centuries, and today, it’s one of the most popular herbal supplements for insomnia. But if you’re already taking a sedative - whether it’s a prescription sleep pill, an anxiety medication, or even just drinking alcohol at night - you might be putting yourself at risk without even knowing it.
What is valerian, and how does it work?
Valerian comes from the root of Valeriana officinalis a flowering plant native to Europe and Asia, long used in traditional medicine for calming nerves and promoting sleep. Unlike synthetic sleep aids, valerian doesn’t knock you out. Instead, it seems to help your brain relax by boosting levels of GABA - a natural chemical that slows down brain activity.
Two key compounds in valerian are believed to be behind this effect: valerenic acid a compound that blocks the enzyme that breaks down GABA, letting more of it build up in the brain, and valepotriates unstable compounds that also have calming effects but degrade quickly during storage. But here’s the catch: not all valerian products are made the same. Some have high levels of valerenic acid, others barely any. And since herbal supplements aren’t regulated like prescription drugs, you can’t always know what you’re actually getting.
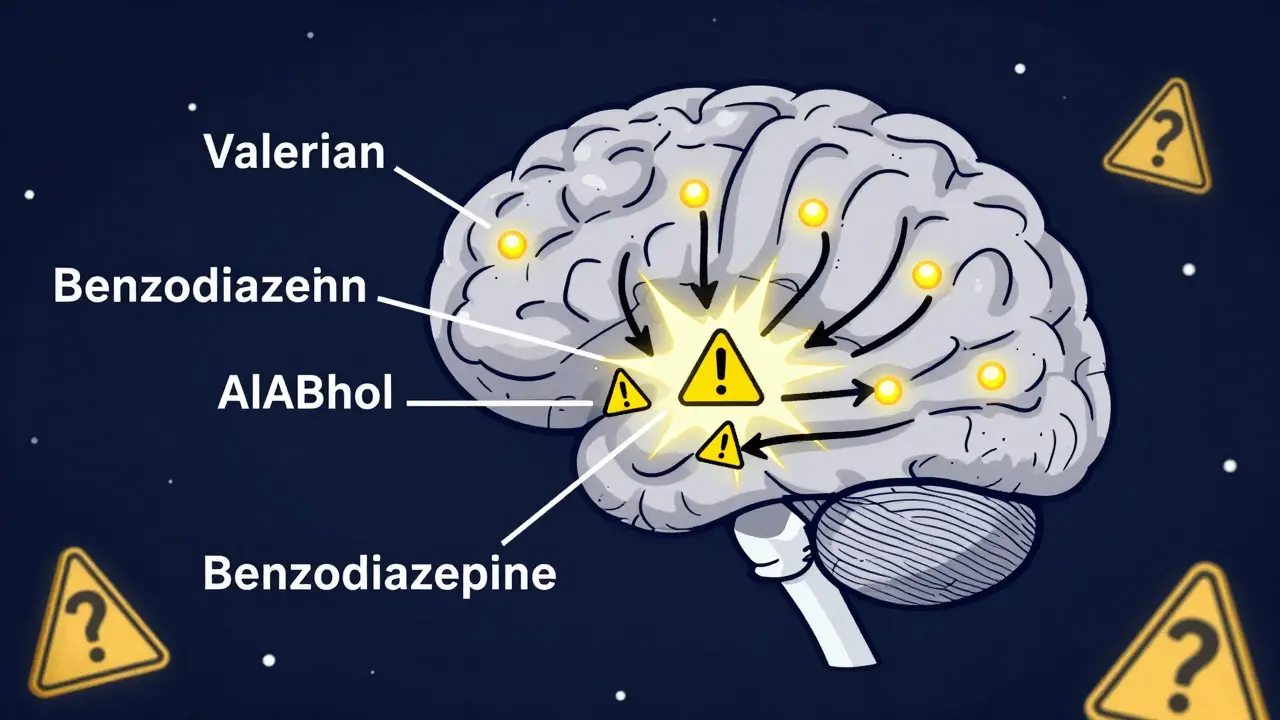
Why combining valerian with sedatives is risky
When you take something that slows down your brain - like alcohol, Xanax, Ambien, or even certain painkillers - your body’s natural ability to stay alert and breathe properly gets reduced. Valerian does the same thing. So when you mix them, you’re stacking two depressants on top of each other.
This is called additive central nervous system (CNS) depression a dangerous condition where brain activity slows too much, leading to extreme drowsiness, dizziness, confusion, slowed breathing, or even loss of consciousness. The risk isn’t theoretical. The NIH Office of Dietary Supplements a trusted U.S. government source warns that valerian "might have additive therapeutic and adverse effects if taken with sedatives." WebMD labels the combination with alcohol and alprazolam (Xanax) as a "Major" interaction - meaning you should avoid it entirely.
Think about this: if you take valerian before bed and also drink a glass of wine, you’re not just doubling the sleepiness. You’re increasing the chance your breathing will slow dangerously. The same goes for benzodiazepines like lorazepam or barbiturates. Even over-the-counter sleep aids containing diphenhydramine can add to the effect.
The science behind the warning
It’s not just guesswork. Studies show valerian increases GABA in the brain. So do most sedative medications. Benzodiazepines (like Xanax or Valium) work by making GABA receptors more sensitive. Barbiturates (like phenobarbital) keep GABA active longer. Alcohol? It enhances GABA too. So when valerian joins the party, it’s like turning up the volume on all those signals at once.
The Mayo Clinic a leading medical authority states clearly: "Valerian may increase the effects of other sleep aids." They also warn it can make you too sleepy if you’re taking narcotics like codeine or oxycodone. And while some people think herbal means safe, the truth is: your body can’t tell the difference between a plant extract and a pill when it comes to how it affects your brain.
What about that 2005 study that says it’s safe?
You might have heard about a 2005 study from Mexico that found valerian didn’t make sedatives stronger in mice. That’s true. But here’s what most people miss:
- The study used Valeriana edulis a different species than the one most people take, not Valeriana officinalis the standard form sold in supplements.
- It was done on mice. Human brains and metabolisms work differently.
- No follow-up human trials have confirmed those results.
That study doesn’t prove valerian is safe with sedatives - it just means we don’t have solid proof it’s dangerous. In medicine, when there’s a plausible risk and serious consequences (like stopped breathing), we err on the side of caution. That’s why every major health organization says: don’t mix them.
Real-world dangers you won’t hear about
Most people don’t think of valerian as a drug. They see it on the shelf next to vitamins and assume it’s harmless. But that’s dangerous.
Consider this: a patient takes valerian before a dental appointment because they’re nervous. They don’t mention it. The dentist gives them nitrous oxide and a local anesthetic. Both are CNS depressants. Now add valerian? The patient could slip into deep sedation, stop breathing, and need emergency intervention. This isn’t a hypothetical. Clinical educators warn that dental professionals often don’t ask about herbal supplements - and patients rarely volunteer the information.
The same goes for surgery. If you’re taking valerian before a procedure and your anesthesiologist doesn’t know about it, they might give you less anesthesia than needed - or worse, too much, because they didn’t account for the extra sedation.

Who’s at highest risk?
You’re especially vulnerable if you:
- Take benzodiazepines (alprazolam, clonazepam, lorazepam)
- Use sleep medications (zolpidem, eszopiclone)
- Drink alcohol regularly, especially at night
- Take opioid painkillers (codeine, hydrocodone, oxycodone)
- Have sleep apnea or other breathing disorders
- Are over 65 - older adults are more sensitive to CNS depression
Even if you’re not on a prescription, if you’re using melatonin, diphenhydramine (Benadryl), or other OTC sleep aids, you’re still at risk.
What should you do?
Here’s the bottom line:
- If you’re on any sedating medication - prescription or not - do not take valerian.
- If you’re already taking valerian and just started a new medication, stop it immediately and talk to your doctor.
- Always tell your doctor and pharmacist about every supplement you take - even "natural" ones.
- If you want to try valerian, do it only after you’ve stopped all other sedatives, and start with the lowest possible dose.
- Don’t use valerian long-term. Persistent insomnia is usually a sign of something else - stress, poor sleep habits, anxiety, or a medical condition.
The NIH says valerian is "generally recognized as safe" when used as directed. But "safe" doesn’t mean "safe with everything." It means safe if you’re not combining it with other brain-slowing substances.
Final thought: Just because it’s herbal doesn’t mean it’s harmless
We live in a world where "natural" is marketed as better, safer, gentler. But nature doesn’t care about your safety. Valerian is powerful. It changes brain chemistry. And when you layer it on top of other drugs that do the same thing, the results can be deadly.
If you’re struggling with sleep, talk to your doctor. There are safer, proven ways to improve rest - without risking your breathing, your safety, or your life.
Can I take valerian with melatonin?
It’s not recommended. Both valerian and melatonin affect your sleep cycle and brain activity. While melatonin doesn’t directly depress the CNS like benzodiazepines, combining it with valerian can still lead to excessive drowsiness, dizziness, or difficulty waking up. If you’re using melatonin for sleep, stick with it alone. Adding valerian increases risk without proven benefit.
How long does valerian stay in your system?
Valerian’s effects usually last 4 to 6 hours, but its compounds can linger in your body longer - up to 12 hours in some people. If you take it at night, you might still feel groggy the next morning. If you’re on a sedative that lasts longer (like some benzodiazepines), the overlap can be dangerous. Always wait at least 12 hours after taking valerian before taking another CNS depressant.
Is valerian safe if I don’t take any other medications?
For most healthy adults without underlying conditions, short-term use of valerian (2-4 weeks) at recommended doses is generally considered safe. But even then, it can cause drowsiness, headaches, or upset stomach. It’s not meant to be a long-term solution. If sleep problems last longer than a few weeks, see a doctor - you may need help addressing the root cause.
Can I take valerian before surgery?
No. You should stop taking valerian at least 2 weeks before any surgery or procedure involving anesthesia. Anesthesiologists need to know exactly how much sedation your body can handle. Valerian can interfere with how anesthesia works, leading to unpredictable effects - including dangerously low blood pressure or breathing problems during surgery.
Are there any supplements that are safer than valerian for sleep?
Magnesium glycinate and glycine are two supplements with strong evidence for improving sleep without significant interaction risks. Unlike valerian, they don’t directly affect GABA receptors or CNS activity. They’re also less likely to interfere with medications. But even these should be discussed with your doctor if you’re on other drugs. The safest approach is always behavioral changes: consistent sleep schedule, dark room, no screens before bed, and managing stress.



Ariel Edmisten
8 February, 2026 . 16:44 PM
I took valerian for a week and felt like a zombie the next day. Just stop. Your body doesn't need another depressant on top of your meds.
Simple as that.
Niel Amstrong Stein
9 February, 2026 . 11:35 AM
Honestly? I get why people do it. 🌿🍷 I'm chill, I take my valerian tea, have a glass of wine, and crash hard. But reading this made me pause. Like... what if I just stop breathing in my sleep? 😅 That’s not a chill vibe anymore. Maybe I’ll switch to magnesium. Less drama, more sleep.
Joey Gianvincenzi
11 February, 2026 . 06:02 AM
The assertion that herbal supplements are inherently safe is not only scientifically unsound but also dangerously irresponsible. The FDA does not regulate these products for purity, potency, or interaction profiles. To conflate 'natural' with 'non-toxic' is a fundamental misunderstanding of pharmacology. This article is not alarmist-it is clinically necessary.
Amit Jain
11 February, 2026 . 15:11 PM
lol u all scared of a plant? we in india have been using valerian for 5000 years with alcohol and no one died. your western medicine is just scared of natural stuff. u take 10 pills and call it science. we take one root and call it wisdom. u scared? good. stay scared.
Sarah B
11 February, 2026 . 17:08 PM
If you take valerian with alcohol you deserve what happens
Savannah Edwards
13 February, 2026 . 08:58 AM
I’ve been on lorazepam for anxiety for 8 years now and I started taking valerian because I thought it would help me sleep deeper without the hangover. It did... but then I started waking up gasping. Like, literally gasping. I thought I was having panic attacks. Turns out it was the combo. I stopped valerian cold turkey and my breathing improved in 3 days. I didn’t even realize how much it was slowing me down. I’m so grateful I read this. I wish I’d known sooner. Don’t wait until you’re almost unconscious to listen. Your body is screaming before it gives up.
Gouris Patnaik
13 February, 2026 . 13:49 PM
You think this is about valerian? No. This is about the collapse of critical thinking. We live in a world where people trust a root more than a doctor because it has a pretty label. The real danger isn’t the herb-it’s the delusion that nature is benevolent. Nature doesn’t care if you live or die. It just exists. You want safety? You want control? Then you need science. Not vibes. Not rituals. Not tea. Science.
Ashley Hutchins
15 February, 2026 . 03:19 AM
I take valerian and wine and i feel so chill its like my brain is on vacation. why would anyone say no to that. you people are too scared of everything. just let urself relax. also i took it with my xanax for 2 years and never had a problem. so your science is prob wrong lol
Lakisha Sarbah
16 February, 2026 . 05:53 AM
I’m a nurse. I’ve seen three patients in the ER this year because they mixed valerian with benzos. One was 72, took it for 'natural sleep' and ended up in intubation. They didn’t even tell their doctor. Please. Just talk to someone. You don’t have to be a hero. Just be smart.
Mary Carroll Allen
17 February, 2026 . 23:02 PM
I tried valerian after my doctor said no to more prescriptions. I thought I was being careful-just a capsule at night. But then I started forgetting my own phone number. Not joking. I’d walk into a room and forget why I was there. I thought I was getting dementia. Turns out it was the valerian + my nightly melatonin. I quit both. My brain came back in 10 days. I feel like myself again. Don’t wait for your mind to vanish before you listen.
Eric Knobelspiesse
19 February, 2026 . 03:21 AM
I get why people do this. I used to. But here’s the thing-valerian doesn’t just add to sedatives. It *warps* them. It’s not 1+1=2. It’s 1+1=5. And your liver doesn’t know the difference between a pill and a root. It just sees 'depressant' and goes 'oh cool, party time.' Your brain doesn’t care if it came from a lab or a forest. It just shuts down. And when it shuts down too hard? No one’s there to hit the reset button.
Heather Burrows
20 February, 2026 . 21:16 PM
I’m not saying this isn’t important. I just... I don’t have the energy to care anymore. Everyone’s so scared of everything. Just take your tea. Take your wine. Take your pills. Do what you want. I’m not your mom. I’m just here reading. And I’m tired.