Lasix vs Other Diuretics Comparison Tool
Select a Diuretic to Compare
Lasix (Furosemide)
Loop Diuretic
Bumetanide
Loop Diuretic
Torsemide
Loop Diuretic
Ethacrynic Acid
Non-Sulfa Loop Diuretic
Hydrochlorothiazide
Thiazide Diuretic
Spironolactone
Potassium-Sparing Diuretic
Comparison Results
Select a diuretic from the list to see detailed comparison information.
Detailed Comparison Table
| Drug | Class | Potency (per mg) | Typical Oral Dose | Renal Clearance | Cost (AU$ per month) |
|---|---|---|---|---|---|
| Lasix (furosemide) | Loop | 1× (baseline) | 20–80 mg | 100–130 mL/min | ≈ $5–$10 |
| Bumetanide | Loop | 1.5–2× | 0.5–2 mg | 80–120 mL/min | ≈ $15–$20 |
| Torsemide | Loop | 1.2–1.5× | 5–20 mg | 90–130 mL/min | ≈ $12–$18 |
| Ethacrynic acid | Loop (non-sulfa) | ≈ 1× | 50–200 mg | 70–110 mL/min | ≈ $20–$30 |
| Hydrochlorothiazide | Thiazide | 0.1× (much milder) | 12.5–50 mg | >150 mL/min | ≈ $3–$8 |
| Spironolactone | Potassium-sparing | 0.05× (very mild) | 25–100 mg | >120 mL/min | ≈ $7–$12 |
Key Points to Remember
- Lasix is the most widely prescribed loop diuretic
- Bumetanide and torsemide are more potent per milligram
- Ethacrynic acid is used for sulfa allergies
- Thiazides and potassium-sparing diuretics are less aggressive
- Choice depends on kidney function, electrolyte balance, and cost
When swelling, high blood pressure, or kidney problems demand a powerful diuretic, most people first think of Lasix comparison. Yet dozens of other drugs can do the job, each with its own strengths and drawbacks. This guide lines up the most common alternatives, breaks down how they differ, and helps you decide which one fits your situation.
Key Takeaways
- Lasix (furosemide) is the most widely prescribed loop diuretic, excellent for rapid fluid removal.
- Bumetanide and torsemide are more potent on a milligram‑for‑milligram basis, often used when patients need stronger diuresis.
- Ethacrynic acid works like a loop diuretic but is reserved for people allergic to sulfonamides.
- Thiazide and potassium‑sparing diuretics are less aggressive; they complement loops or stand alone for mild hypertension.
- Kidney function, electrolyte balance, and cost are the three biggest factors in choosing the right drug.
What is Lasix (Furosemide)?
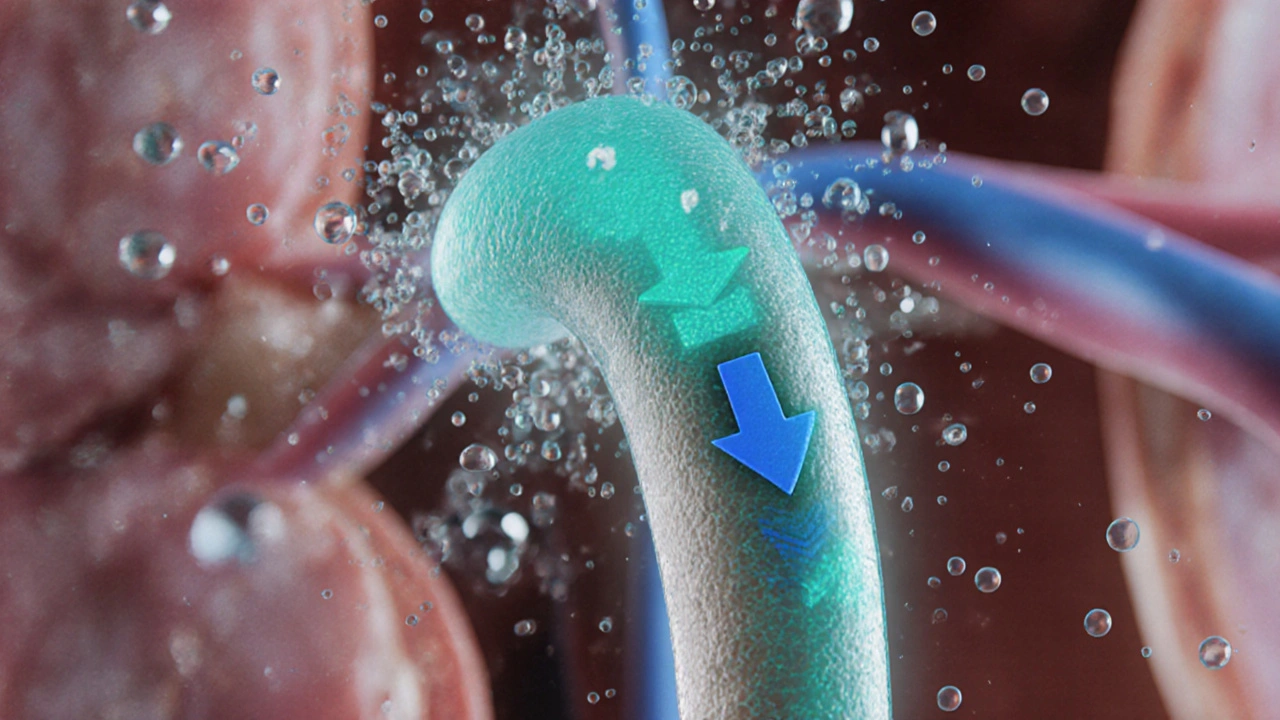
Lasix is the brand name for furosemide, a high‑potency loop diuretic introduced in 1966. It works by blocking the Na‑K‑2Cl co‑transporter in the thick ascending limb of the loop of Henle, forcing the kidneys to excrete sodium, chloride, and water.
How Lasix Works
By inhibiting that transporter, Lasix reduces reabsorption of about 25% of filtered sodium. The resulting increase in urine output clears excess fluid from the lungs, legs, and abdomen. Because it acts early in the nephron, the electrolyte loss can be significant, so patients often need potassium supplements or a potassium‑sparing partner.
Typical Uses and Dosing
- Edema from heart failure, liver cirrhosis, or nephrotic syndrome - starting dose 20‑40mg orally or IV, titrated to effect.
- Acute pulmonary edema - rapid IV bolus of 40‑80mg, repeat as needed.
- Hypertension that resists other agents - low‑dose oral regimen (12.5‑25mg) once or twice daily.
Major Side Effects & Cautions
Common issues include dehydration, low potassium (hypokalemia), low sodium (hyponatremia), and a rise in uric acid that can trigger gout attacks. Rare but serious risks are ototoxicity (hearing loss) at high IV doses and severe allergic reactions. Patients with an eGFR below 30mL/min/1.73m² need dose adjustments and close monitoring.
Alternatives to Lasix
Below are the most frequently prescribed loop and non‑loop diuretics that clinicians consider when Lasix isn’t a perfect fit.
Bumetanide is a loop diuretic about 40% more potent than furosemide, often used in patients who need a smaller pill size.
Torsemide offers a smoother, longer‑lasting diuresis and may cause fewer electrolyte swings.
Ethacrynic acid is a non‑sulfonamide loop diuretic, reserved for sulfa‑allergic patients.
Hydrochlorothiazide belongs to the thiazide class; it’s milder, ideal for low‑dose hypertension control.
Spironolactone is a potassium‑sparing diuretic that counters the potassium loss caused by loops and thiazides.

Side‑by‑Side Comparison
| Drug | Class | Potency (per mg) | Typical Oral Dose | Renal Clearance | Cost (AU$ per month) |
|---|---|---|---|---|---|
| Lasix (furosemide) | Loop | 1× (baseline) | 20‑80mg | 100‑130mL/min | ≈$5‑$10 |
| Bumetanide | Loop | 1.5‑2× | 0.5‑2mg | 80‑120mL/min | ≈$15‑$20 |
| Torsemide | Loop | 1.2‑1.5× | 5‑20mg | 90‑130mL/min | ≈$12‑$18 |
| Ethacrynic acid | Loop (non‑sulfa) | ≈1× | 50‑200mg | 70‑110mL/min | ≈$20‑$30 |
| Hydrochlorothiazide | Thiazide | 0.1× (much milder) | 12.5‑50mg | >150mL/min | ≈$3‑$8 |
| Spironolactone | Potassium‑sparing | 0.05× (very mild) | 25‑100mg | >120mL/min | ≈$7‑$12 |
How to Choose the Right Diuretic
Three practical questions guide the decision:
- How severe is the fluid overload? For rapid, large‑volume removal, a loop diuretic (Lasix, bumetanide, torsemide) is first‑line. If the excess is modest, a thiazide or low‑dose loop may suffice.
- What is the patient’s kidney function? In chronic kidney disease (eGFR <30), loop potency drops, and doses need careful tweaking. Some clinicians favor torsemide because its longer half‑life offers steadier control.
- Are there allergy or electrolyte concerns? Sulfa‑allergic patients should avoid furosemide, bumetanide, and torsemide; ethacrynic acid becomes the loop of choice. If potassium loss is a problem, add spironolactone or switch to a thiazide‑loop combo.
Cost is also a factor in Australia. Generic furosemide remains the cheapest, while torsemide and ethacrynic acid can be pricey without PBS (Pharmaceutical Benefits Scheme) subsidy.
Practical Tips for Safe Use
- Measure weight daily; a 1‑kg drop usually means a liter of fluid loss.
- Check serum potassium at baseline and after the first week of therapy.
- Stay hydrated with oral fluids unless the doctor orders strict fluid restriction.
- Set reminders for dose timing; most loops are taken twice daily for steady effect.
- If you hear ringing in the ears after a high IV dose, call your health provider immediately - it may signal ototoxicity.
Frequently Asked Questions
Can I switch from Lasix to a cheaper generic?
Yes. In Australia, generic furosemide is widely available and costs only a few dollars per month. Always discuss the switch with your prescriber to confirm the dose conversion.
Why does Lasix sometimes cause low potassium?
Because it forces the kidneys to dump sodium and water, potassium follows the same route. Many doctors add a potassium supplement or pair Lasix with spironolactone to keep levels stable.
Is torsemide better for heart‑failure patients?
Research from 2022 shows torsemide improves symptoms and reduces hospital readmissions compared with furosemide in some heart‑failure cohorts, likely because of its longer duration and more predictable absorption.
What should I do if I miss a dose?
Take the missed dose as soon as you remember unless it’s almost time for the next one. Never double‑dose; that can cause a sudden drop in blood pressure and severe electrolyte loss.
Are there any foods I should avoid while on Lasix?
Limit high‑salt foods, as they counteract the drug’s effect. Also watch out for grapefruit juice, which can increase plasma levels of some loop diuretics.
Choosing between Lasix and its alternatives isn’t a one‑size‑fits‑all decision. By weighing fluid‑removal needs, kidney health, allergy status, and cost, you can land on the diuretic that keeps swelling at bay without unwanted side effects.





Satyabhan Singh
7 October, 2025 . 16:43 PM
When contemplating diuretic therapy, one must first consider the epistemological foundations of pharmacology. The ancient physicians of Ayurveda recognized the value of fluid balance long before the advent of synthetic loop diuretics. Modern medicine, however, quantifies that balance through precise metrics such as renal clearance and electrolyte homeostasis. Lasix, as the archetype of loop diuretics, provides a rapid reduction in extracellular volume, a fact well‑documented in countless clinical trials. Yet potency alone does not confer superiority; the physician must weigh potency against potential iatrogenic disturbances. For a patient with compromised kidney function, a drug with a modest potency but favorable safety profile may be preferable. Bumetanide’s higher milligram potency can be advantageous when pill burden is a concern, but it also carries a steeper risk of ototoxicity at high intravenous doses. Torsemide offers a smoother pharmacokinetic curve, often resulting in fewer abrupt electrolyte shifts. Ethacrynic acid, while chemically similar, avoids sulfonamide allergies, illustrating how structural nuances dictate clinical choices. Thiazide diuretics, such as hydrochlorothiazide, act upstream in the distal convoluted tubule and are therefore less powerful but useful for hypertension control. Spironolactone, by antagonizing aldosterone, preserves potassium, mitigating the hypokalemia commonly induced by loops. Cost considerations, although seemingly trivial, influence adherence, especially in health systems with out‑of‑pocket expenses. Cultural perceptions of medication also play a role; some communities distrust “strong” diuretics, preferring gentler agents. Consequently, the selection of a diuretic is an exercise in balancing pharmacodynamic potency, renal physiology, patient comorbidities, economic factors, and cultural acceptance. Ultimately, the physician’s duty is to tailor therapy to the individual, guided by both evidence and empathy.
Keith Laser
8 October, 2025 . 14:03 PM
Oh sure, just pick the cheapest loop and hope for the best – because who needs nuanced dosing?
Winnie Chan
9 October, 2025 . 11:26 AM
I get it, you want the “biggest hammer” for a little dent, but sometimes a thiazide does the trick without the drama.
Kyle Rensmeyer
10 October, 2025 . 08:50 AM
Lasix works fast 😏 but watch those electrolytes 😬
Rod Maine
11 October, 2025 . 06:13 AM
Yo the loop thingy is rite but the price is high
Othilie Kaestner
12 October, 2025 . 03:36 AM
As an American, we love a good high‑potency diuretic, but let’s not forget the side‑effects that keep our healthcare spending soaring.
Sebastian Samuel
13 October, 2025 . 01:00 AM
💊 Lasix = fast fluid loss, 💸 cheap, 👍 but mind the potassium drop! 😅
Mitchell Awisus
13 October, 2025 . 22:23 PM
When you consider the pharmacokinetic profile of Lasix, you’ll notice that its half‑life is relatively short, which can be both an advantage and a drawback, depending on the clinical scenario, and that’s why many clinicians pair it with a potassium‑sparing agent.
Annette Smith
14 October, 2025 . 19:46 PM
A diuretic is just a tool; it’s how we use it that defines its value.
beth shell
15 October, 2025 . 17:10 PM
Choosing a diuretic is personal and depends on health and cost
khushali kothari
16 October, 2025 . 14:33 PM
From a nephrological standpoint, the GFR‑dependent clearance of loop agents necessitates dosage titration based on fractional excretion of sodium, thereby ensuring euvolemia while mitigating iatrogenic hypovolemia.
Brandon Smith
17 October, 2025 . 11:56 AM
It’s disgraceful that anyone would ignore the well‑established guidelines and prescribe a cheap loop without monitoring electrolytes-patient safety must come first.
darwin ambil
18 October, 2025 . 09:20 AM
Haha, anyone tried swapping Lasix for bumetanide? 😂 It’s tiny but mighty! 🙌
Kelvin Van der Maelen
19 October, 2025 . 06:43 AM
Wow, look at you bragging about the most potent pill, think you’re a superhero!
Joy Arnaiz
20 October, 2025 . 04:06 AM
One must question whether the pharmaceutical conglomerates are deliberately promoting certain diuretics to maximize profit margins, subtly steering clinical practice away from older, less expensive alternatives.
Christopher Eyer
21 October, 2025 . 01:30 AM
Actually the data shows no such conspiracys, the guidelines are evidence‑based, even if they sometimes look like marketing.