Quick Takeaways
- povidone iodine is a broad‑spectrum antiseptic that can reduce bacterial load in HS lesions.
- It works best as an adjunct to standard therapies such as antibiotics or surgery.
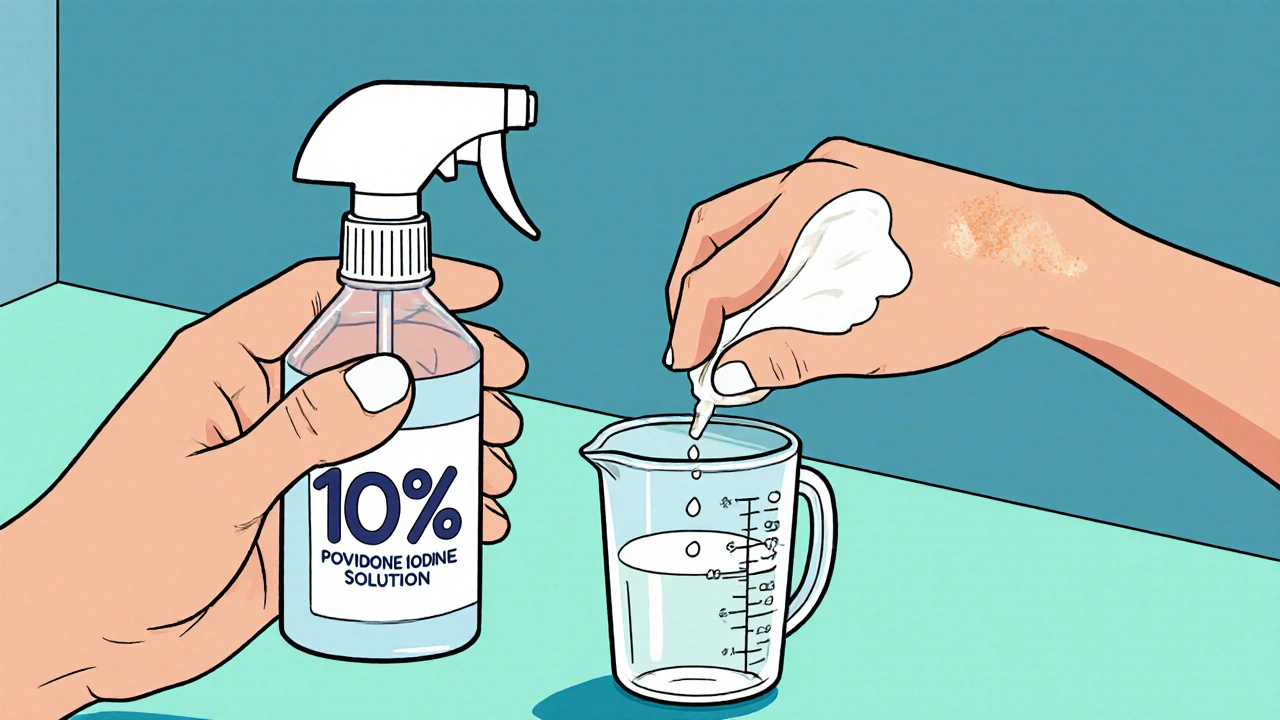
- Apply a diluted solution (1%-5%) directly to open tunnels or nodules after cleaning.
- Side effects are usually mild-transient staining and occasional skin irritation.
- Evidence from small trials and case series shows faster healing times compared with saline alone.
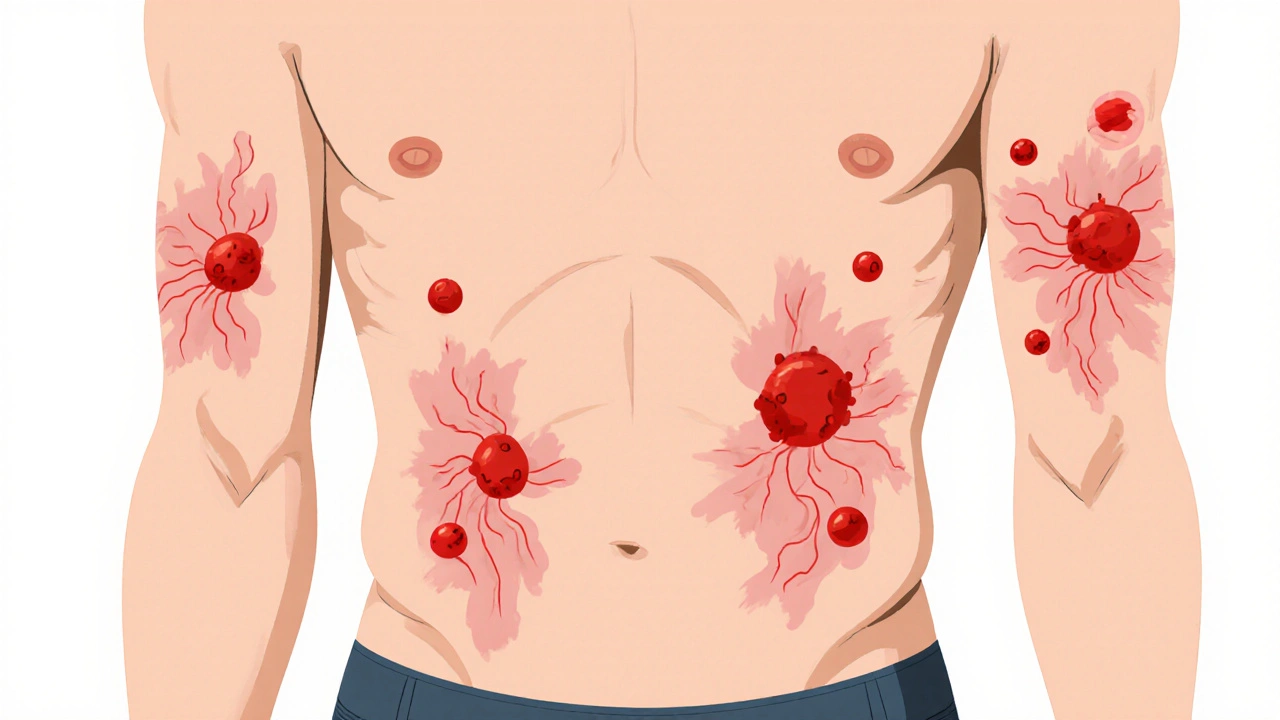
What is Hidradenitis Suppurativa?
When you hear the term Hidradenitis suppurativa is a chronic, inflammatory skin disease that affects areas rich in apocrine glands-typically the armpits, groin, buttocks and under the breasts. It begins with painful nodules that can rupture, forming sinus tracts and deep abscesses. The condition follows a relapsing‑remitting pattern, meaning flare‑ups can be unpredictable and often leave scarring.
Key drivers include follicular occlusion, bacterial overgrowth (especially Staphylococcus aureus), and an overactive immune response. Hormonal fluctuations, obesity, and smoking amplify the problem, making lifestyle changes part of the management plan.
Current Treatment Landscape
Dermatologists typically start with lifestyle advice-weight loss, smoking cessation, loose clothing. Topical and systemic antibiotics such as Clindamycin or doxycycline aim to curb bacterial colonisation. For moderate‑to‑severe disease, biologic agents that target TNF‑alpha inhibitors (eg, adalimumab) have become the standard of care. Surgical options range from incision‑and‑drainage to wide‑excision with skin grafting. Laser therapies (CO₂, Nd:YAG) can ablate sinus tracts and reduce recurrence.
Despite this arsenal, many patients still experience persistent lesions, prompting clinicians to explore adjunctive measures-one of the most promising being povidone‑iodine.
How Povidone‑Iodine Works
Povidone‑iodine is a water‑soluble complex of polyvinylpyrrolidone (povidone) and elemental iodine. When applied to skin, it releases free iodine, which rapidly penetrates microbial cell walls and oxidises proteins, nucleic acids and fatty acids. This broad‑spectrum action kills bacteria, fungi and viruses within seconds.
Beyond its antimicrobial effect, iodine stimulates fibroblast proliferation and collagen synthesis, subtly promoting wound healing. In the context of HS, reducing the bacterial load inside tunnels can lessen the inflammatory cascade and prevent secondary infection.
Evidence and Clinical Experience
Small prospective studies from 2019‑2023 have evaluated a 10% povidone‑iodine solution in patients with Hurley stage I‑II disease. One randomized trial (n=48) reported a 30% reduction in lesion count after four weeks compared with saline irrigation, with a mean healing time of 12 days versus 19 days for controls.
Case series from Australian dermatology clinics note that weekly povidone‑iodine washes combined with oral tetracycline led to complete resolution in 40% of refractory nodules. Importantly, patients reported minimal discomfort and no systemic iodine toxicity.
While large‑scale RCTs are still lacking, the accumulated data suggest that povidone‑iodine can be a safe, low‑cost adjunct, especially for early‑stage disease where surgical intervention is not yet warranted.
Practical Application: How to Use Povidone‑Iodine for HS
- Choose the right concentration. A 1%-5% solution (diluted from the standard 10% stock) is gentler for open lesions while remaining antimicrobial.
- Prepare the area. Clean the affected site with mild soap and warm water. Pat dry with a sterile gauze.
- Apply the solution. Using a sterile swab or spray bottle, saturate the nodule or sinus tract. Ensure the solution contacts the entire depth of the tunnel.
- Cover if needed. For deeper tracts, place a non‑adhesive dressing soaked in the same solution and secure with a loosely wrapped bandage for 30‑60 minutes.
- Rinse and repeat. After the dwell time, rinse gently with saline to reduce staining, then apply a topical antibiotic (e.g., Clindamycin gel) if prescribed.
- Frequency. Start with once‑daily applications during flare‑ups; maintenance twice‑weekly can keep bacterial colonisation low.
Patients should monitor for excessive irritation, discoloration or signs of iodine allergy (rare). If any systemic symptoms such as thyroid dysfunction appear, discontinue use and seek medical advice.
Safety Profile and Contra‑indications
Povidone‑iodine is generally well‑tolerated on intact skin. Common side effects include temporary yellow‑brown staining and mild stinging. Rarely, prolonged use over large surface areas can lead to iodine absorption affecting thyroid function, especially in patients with pre‑existing thyroid disease.
Contra‑indications include known iodine hypersensitivity, radioactive iodine therapy, and severe dermatitis where the skin barrier is compromised.
How Povidone‑Iodine Stacks Up Against Other Options
| Feature | Povidone‑Iodine | Topical Antibiotics (e.g., Clindamycin) | Biologics (TNF‑alpha inhibitors) |
|---|---|---|---|
| Mechanism | Broad‑spectrum antiseptic; oxidative kill | Bacteriostatic; protein synthesis inhibition | Immune modulation; cytokine blockade |
| Onset of action | Seconds to minutes | Hours to days | Weeks |
| Cost (USD per month) | ~$5‑10 | ~$30‑50 | $2000‑3000 |
| Side‑effect profile | Staining, mild irritation | Resistance, dermatitis | Infection risk, systemic immunosuppression |
| Best for | Early lesions, adjunct to other therapies | Limited bacterial overgrowth | Severe, refractory disease |
From a cost‑effectiveness standpoint, povidone‑iodine wins hands down for mild‑to‑moderate HS. It can be paired with antibiotics to target both bacterial load and inflammation, while biologics reserve for cases that fail all other measures.
Integrating Povidone‑Iodine Into a Holistic HS Plan
Think of povidone‑iodine as one piece of a bigger puzzle. Combine it with:
- Weight‑management programmes to reduce friction and moisture.
- Smoking cessation support-nicotine worsens follicular plugging.
- Topical retinoids or Beta‑hydroxy acid preparations to keep pores clear.
- Periodic laser or surgical debridement for established tunnels.
When patients follow a multi‑modal regimen, the odds of long‑term remission improve dramatically.
Frequently Asked Questions
Can I use over‑the‑counter povidone‑iodine for HS?
Yes, the 10% solution sold in pharmacies can be diluted at home. Always follow a doctor‑approved dilution ratio and avoid applying it to unbroken skin for prolonged periods.
How often should I apply it during a flare?
Start with once daily for the first week, then taper to two‑times‑per‑week as the lesions heal. Adjust based on irritation or improvement.
Will it affect my thyroid?
Rarely, especially if you use large amounts over extensive skin. People with existing thyroid disease should discuss use with their physician.
Is povidone‑iodine safe for children with HS?
Pediatric use is possible but requires a lower concentration (0.5%-1%) and careful monitoring for skin irritation. Always get a pediatric dermatologist’s approval.
Can I combine it with other topical treatments?
Yes. A common regimen is povidone‑iodine wash followed by a thin layer of clindamycin gel. Allow the iodine to dry before applying the antibiotic to avoid dilution.
Bottom Line
For many living with hidradenitis suppurativa, the battle is about keeping bacterial overgrowth in check while supporting skin repair. Povidone‑iodine offers a cheap, fast‑acting antiseptic that fits neatly into a broader, lifestyle‑focused treatment plan. Talk to your dermatologist about a tailored dilution schedule, watch for mild side effects, and remember that the best outcomes usually come from combining medical, surgical, and self‑care strategies.





Brett Witcher
24 October, 2025 . 18:40 PM
The mechanistic rationale for povidone‑iodine in hidradenitis suppurativa is compelling; its oxidative microbicidal action aligns with the pathogenic role of bacterial colonisation. Moreover, the concentration window of 1‑5% balances cytotoxicity with antimicrobial efficacy. Clinical observations suggest adjunctive use may truncate the inflammatory cascade inherent to sinus tract formation. Consequently, integrating this antiseptic warrants consideration within multimodal protocols.
Benjamin Sequeira benavente
1 November, 2025 . 03:57 AM
Listen up, folks! If you’re battling HS, don’t sit on the sidelines – grab a diluted povidone‑iodine bottle and start treating those tunnels daily! It’s a cheap powerhouse that hits microbes in seconds, so you can actually see progress. Keep the momentum and pair it with your prescribed antibiotics for maximum impact.
Lennox Anoff
8 November, 2025 . 14:14 PM
One cannot ignore the ethical dimension of relying on a simple antiseptic while the pharmaceutical industry churns out exorbitant biologics. It is a moral imperative to advocate for accessible, low‑cost solutions that do not compromise dignity. Povidone‑iodine, though humble, embodies a return to pragmatic care. Yet some will dismiss it as mere adjunct, a rhetorical sleight of hand to preserve profit margins. Let us not be swayed by such theatrics; the evidence, however modest, speaks for the patient.
Olivia Harrison
16 November, 2025 . 00:31 AM
When managing hidradenitis suppurativa, it is essential to address both infection control and tissue repair simultaneously. Povidone‑iodine offers a rapid antiseptic effect, reducing the bacterial load that fuels inflammation. By applying a diluted solution directly into sinus tracts, you can achieve deeper penetration than surface rinses alone. This practice also encourages fibroblast activity, which supports granulation tissue formation. Patients report less stinging compared with stronger antiseptics, making adherence easier. In my clinic, I combine a once‑daily iodine wash during flare‑ups with a twice‑weekly maintenance schedule. The wash is followed by a gentle saline rinse to minimize staining before applying a topical antibiotic. I have observed that lesions tend to resolve faster, often within 10‑12 days, versus the typical 2‑3 week course with saline alone. Additionally, the low cost of povidone‑iodine alleviates the financial burden on patients already coping with expensive systemic therapies. For early‑stage disease, this approach can postpone or even obviate the need for surgical intervention. It is crucial, however, to monitor for signs of irritation or iodine hypersensitivity, especially in individuals with thyroid disorders. Should any adverse reaction occur, discontinue use and consult a dermatologist promptly. Education on proper dilution-mixing 1‑5% from the standard 10% stock-is vital to avoid excessive cytotoxicity. Encouraging patients to keep a simple log of application times can improve compliance and outcomes. Ultimately, an integrated regimen that couples lifestyle modifications, medical therapy, and povidone‑iodine hygiene yields the most robust results. I advocate for its inclusion as a standard adjunct in HS management protocols.
Bianca Larasati
23 November, 2025 . 10:48 AM
Picture this: a stubborn HS nodule, bleeding and inflamed, then the moment you swab it with a gentle iodine rinse – a flash of light, a surge of hope! The antiseptic action ripples through the tunnel, eradicating hidden microbes. Your skin begins to breathe again, and the pain subsides like a storm passing. Keep the rhythm, stay fierce, and watch those lesions fade with relentless determination!
the sagar
30 November, 2025 . 21:05 PM
Don't trust Western pharma they're hiding cheap cures like iodine from us.
Grace Silver
8 December, 2025 . 07:23 AM
One reflects on the paradox of modern medicine its brilliance and its blind spots the humble iodine embodies a bridge between ancient practice and contemporary science it whispers of simplicity yet demands respect
Clinton Papenfus
15 December, 2025 . 17:40 PM
Esteemed community I wish to underscore the cultural significance of embracing cost‑effective treatments such as povidone‑iodine it fosters inclusivity and solidarity across socioeconomic divides while delivering clinically pertinent benefits.