Bridging Therapy Calculator
This tool determines if bridging therapy is medically necessary based on current guidelines (AHA 2020). Bridging therapy is ONLY recommended for very high-risk cases.
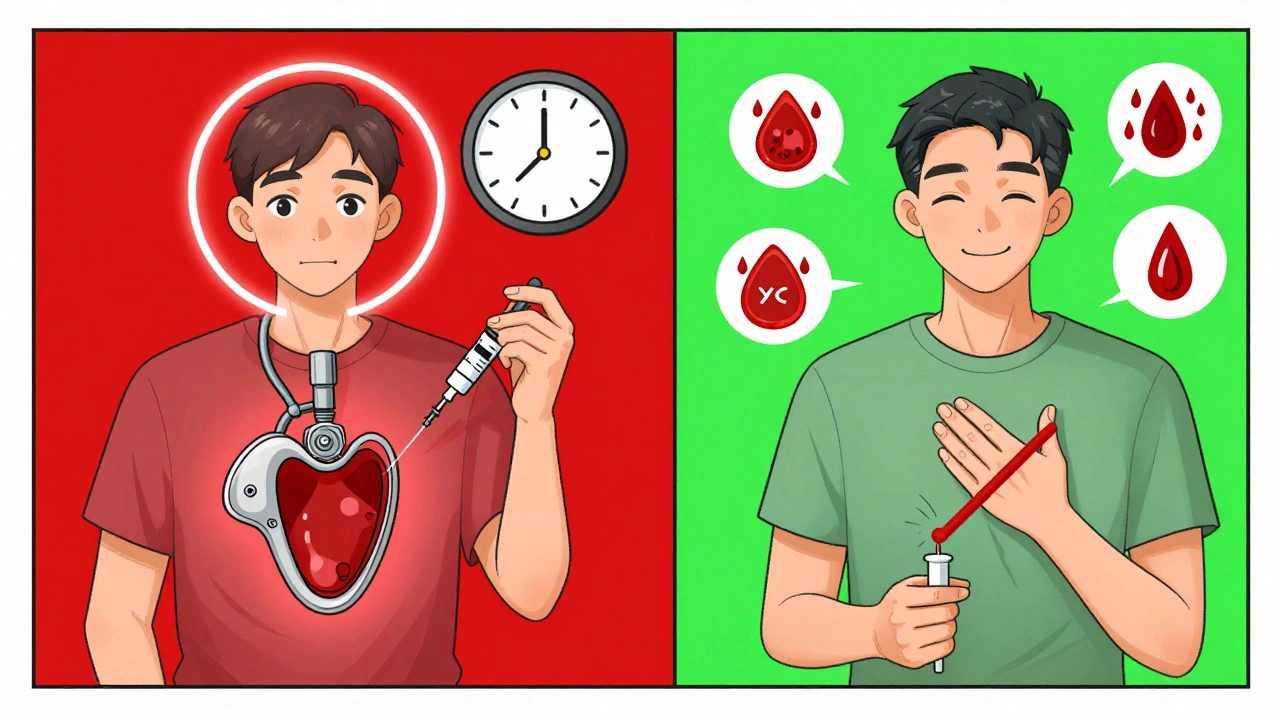
Switching between blood thinners isn’t something you do on a whim. It’s a high-stakes decision that can mean the difference between a clot forming and a dangerous bleed. If you’re on warfarin and need surgery, a dental procedure, or any kind of invasive treatment, your doctor might talk about bridging therapy. But here’s the thing: for most people, bridging isn’t needed anymore. And if you’re on one of the newer blood thinners, you probably don’t need it at all.
What Is Bridging Therapy, Really?
Bridging therapy means using a short-acting injectable blood thinner-like low molecular weight heparin (LMWH), such as enoxaparin (Lovenox)-to temporarily replace your regular blood thinner when you have to stop it. The goal? Keep your blood from clotting during the time your main medication is turned off. This used to be standard practice. Back in the 2000s, if you were on warfarin and needed a procedure, doctors would stop your pill a week before and start you on daily injections. The idea was simple: don’t leave you unprotected. But in 2015, the BRIDGE trial changed everything. Researchers looked at over 1,800 patients with atrial fibrillation who were on warfarin and needed surgery. Half got bridging with LMWH. The other half didn’t. The results? Bridging didn’t lower the risk of stroke or clots. But it doubled the chance of major bleeding-2.3% versus 1%. That’s not a small trade-off. It’s a clear signal: for most people, the risk of bleeding outweighs the benefit of bridging.When Do You Actually Need Bridging?
Not everyone. In fact, only a small group still needs it. The current guidelines (from the American Heart Association, 2020) say bridging is only recommended for people with very high risk of clots. That means:- People with a mechanical heart valve in the mitral position
- People who had a blood clot in their lung or leg within the last 3 months
Warfarin vs. DOACs: Why One Needs Bridging and the Other Doesn’t
This is where things get simple if you understand how the drugs work. Warfarin takes days to build up in your system and days to leave it. That’s why you have to stop it 5-6 days before surgery. Your INR (a blood test that measures clotting time) has to drop below 1.5 before the procedure. That leaves a gap where you’re unprotected-hence the need for bridging in high-risk cases. DOACs-like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa)-work differently. They kick in within hours and leave your body in 12-48 hours, depending on your kidney function. That means:- You stop your DOAC 24-48 hours before surgery (sometimes even less, depending on the procedure)
- You restart it 12-24 hours after, once bleeding risk is low
- You don’t need injections. You don’t need bridging.
How Bridging Works: The Timing Matters
If you’re one of the few who need bridging, timing is everything. Get it wrong, and you risk clotting or bleeding. Here’s the standard protocol for warfarin patients needing bridging:- Stop warfarin 5-6 days before surgery.
- Check your INR 1-2 days before stopping-it should be below 2.0 to start bridging safely.
- Start LMWH (like Lovenox) 24-48 hours after the last warfarin dose.
- Give LMWH twice daily at therapeutic dose (usually 1 mg/kg).
- Stop LMWH 24 hours before surgery.
- Restart warfarin 12-24 hours after surgery, often at 15-20% higher than your previous daily dose.
- Check INR 3-4 days after restarting.
The Hidden Costs of Bridging
It’s not just about bleeding risk. Bridging is expensive and inconvenient. A 7-day course of LMWH costs between $300 and $500 in the U.S. without insurance. You have to inject yourself-usually twice a day. Many patients struggle with this. Studies show 15-20% don’t follow the injection schedule correctly. Some skip doses. Others inject at the wrong time. That increases both clot and bleeding risks. There’s also the mental toll. Worrying about shots, timing, bleeding, and when to restart your pill adds stress to an already stressful time-preparing for surgery. And here’s the kicker: if you’re on a DOAC, you avoid all of this. No shots. No INR checks. No bridging. Just stop, wait, restart. Simpler. Safer.What About After the Procedure?
Restarting your blood thinner after surgery is just as important as stopping it. For warfarin patients on bridging:- Restart warfarin 12-24 hours after surgery
- Use a slightly higher dose (15-20% above your usual) to get back to therapeutic levels faster
- Check INR in 3-4 days
- Stop LMWH once your INR is above 2.0
- Restart 12-24 hours after low-risk procedures (like colonoscopy or cataract surgery)
- Wait 48-72 hours after major surgery (like hip replacement or open-heart surgery)
- Restart only when bleeding risk is low-your surgeon will tell you
Why Doctors Are Changing Their Minds
Ten years ago, bridging was routine. Now, it’s rare. The BRIDGE trial (2015) and the PERIOP2 trial (2020) showed no benefit-only harm. The American College of Cardiology, the American Heart Association, and the American College of Chest Physicians all updated their guidelines to reflect this. The message is clear: Don’t bridge unless you absolutely have to. Dr. James Douketis, lead researcher of the BRIDGE trial, said it best: “Perioperative bridging anticoagulation with LMWH in patients with atrial fibrillation... did not significantly reduce the risk of arterial embolism but significantly increased the risk of major bleeding.” Many doctors still default to bridging out of habit. But the evidence is in. If your doctor suggests bridging and you don’t have a mechanical mitral valve or a recent clot, ask: “Is this really necessary?”What You Can Do to Stay Safe
If you’re on a blood thinner and have a procedure coming up:- Know which one you’re taking-warfarin or a DOAC?
- Ask your doctor: “Am I at high risk for clots? Do I need bridging?”
- Make sure your INR is checked before stopping warfarin.
- Ask if you can switch to a DOAC before your procedure-it might eliminate the need for bridging altogether.
- Write down your medication schedule and share it with your surgeon and pharmacist.
- Don’t stop or restart your meds on your own.
What’s Next for Blood Thinners?
The future is clear: fewer warfarin users. More DOACs. Less bridging. DOACs are safer, easier, and more predictable. They don’t need regular blood tests. They don’t interact with food the way warfarin does. And they don’t require injections. As more people switch, bridging therapy will become a relic of the past-used only in rare, high-risk cases. If you’re still on warfarin and need a procedure, talk to your doctor about switching to a DOAC. It might make your next surgery safer, simpler, and less stressful.It’s not about doing more. It’s about doing less-only what’s truly necessary.




Ashley Farmer
8 December, 2025 . 05:42 AM
I had to switch from warfarin to Eliquis last year before my knee surgery, and honestly? It was a game-changer. No shots, no daily INR checks, no panic about bleeding. Just stop it a day before, do the surgery, restart it the next day. So much less stressful.
My old doctor kept pushing bridging like it was gospel, but my new cardiologist laughed and said, 'You’re not on a mechanical valve-why are we doing this?'
Jennifer Anderson
9 December, 2025 . 18:20 PM
omg i didnt even know bridging was a thing until my mom had to do it last year. she was on warfarin and they made her do lovenox shots twice a day for a week. she cried every time she had to inject herself. i was like… why??
turns out she didnt even need it. my aunt got the same surgery 6 months later on a doac and just stopped her pill for 24hrs. no drama. no needles. no stress.
Sadie Nastor
11 December, 2025 . 08:09 AM
thank you for this!! 🙏
i’ve been on Xarelto for 3 years and my last dentist appointment was a breeze-no stopping, no bridging, just a quick ‘hold your pill today’ note. i always assumed everyone had to go through the whole ‘injection nightmare’ like in the 2010s.
so glad medicine is finally catching up. i feel like i got lucky without even trying 😅
Sangram Lavte
12 December, 2025 . 03:20 AM
As a physician in India, I’ve seen this shift firsthand. Warfarin is still common here due to cost, but when patients can afford DOACs, the outcomes are dramatically better. Bridging isn’t just unnecessary-it’s a logistical nightmare in resource-limited settings.
Many patients miss doses of LMWH because they can’t afford the refrigeration or don’t have access to trained nurses. The risk-benefit ratio is even worse here than in the US.
Oliver Damon
12 December, 2025 . 05:35 AM
The paradigm shift here is epistemological as much as clinical. The BRIDGE trial didn’t just challenge a protocol-it dismantled a deeply entrenched heuristic: ‘Better safe than sorry.’
But ‘safe’ in anticoagulation isn’t binary. It’s a dynamic equilibrium between thrombotic and hemorrhagic risks. Bridging was a crude heuristic that assumed uniform risk profiles across heterogeneous populations. DOACs, with their predictable pharmacokinetics, allow for precision anticoagulation-eliminating the need for population-level over-treatment.
This is a textbook case of evidence-based medicine replacing tradition with biostatistics.
Ernie Blevins
13 December, 2025 . 14:24 PM
So now they’re telling us the whole system was a scam? Doctors were just injecting people for money? That’s why my insurance denied my Lovenox last year-said ‘not medically necessary.’
Wait, so all those years I was getting shots… I was being used? I’m not mad, I’m just disappointed.
David Brooks
15 December, 2025 . 04:07 AM
THIS IS THE MOST IMPORTANT POST I’VE READ ALL YEAR. 🙌
I almost got bridged last month for a colonoscopy. My doctor said, ‘We always do it.’ I said, ‘Wait-what’s the evidence?’ He paused. Then said, ‘You’re right. Let’s just hold your pill.’
Thank you for giving me the courage to ask. I’m telling everyone I know.
Nicholas Heer
15 December, 2025 . 10:52 AM
you think this is about science? nah. big pharma pushed DOACs because they make 10x the profit. they paid off the AHA, the ACC, the FDA-everyone. now they want you to stop warfarin so you’re stuck paying $500/month for Eliquis.
and don’t get me started on how they ‘accidentally’ stopped funding warfarin clinics. they want you dependent. this is capitalism, folks.
Kurt Russell
15 December, 2025 . 20:09 PM
LET’S GOOOOO! 🚀
This is why I love modern medicine. No more needles. No more panic INR checks. No more ‘oh wait, you need to stop your pill 6 days before?’
If you’re still on warfarin and you’re not a mechanical valve patient-SWITCH. Your future self will hug you. I switched in 2021 and haven’t looked back. Life is too short for injections and stress.
Kyle Flores
17 December, 2025 . 13:46 PM
My grandma was on warfarin for 12 years. She had a stroke last year and they switched her to Pradaxa. She didn’t even know she was eligible. No one told her.
Now she’s back to gardening, no shots, no blood tests. She says she feels like she got her life back.
If you’re on warfarin and you’re not in the high-risk group? Ask your doctor about switching. It’s not just easier-it’s safer.
Ryan Sullivan
19 December, 2025 . 00:06 AM
While the data is compelling, one must acknowledge the cognitive dissonance inherent in abandoning a protocol that has been codified for decades. The inertia of clinical practice is not easily overcome by randomized trials alone. Moreover, the generalizability of BRIDGE to non-Western, non-tertiary care settings remains underexplored.
Additionally, the financial incentives driving DOAC adoption may be conflated with clinical superiority. One must remain vigilant against the commodification of medical knowledge.
Louis Llaine
19 December, 2025 . 02:12 AM
so let me get this straight… you’re telling me the whole ‘bridging’ thing was just doctors being lazy and scared to do less?
and now they’re patting themselves on the back for not killing people?
congrats, you finally stopped doing something stupid. take a medal.
Jane Quitain
19 December, 2025 . 16:04 PM
i switched to Eliquis last year and it was so easy. i forgot to stop it one day before my dental cleaning and they still did it. no big deal. no shots. no panic.
my mom still does the lovenox thing and she’s like ‘but what if i bleed?’ i’m like… you’re more likely to bleed from the shots than the surgery lol.
Kyle Oksten
20 December, 2025 . 20:14 PM
The real question isn’t whether bridging works-it’s why we ever thought it did. We treated anticoagulation like a binary switch: on or off. But the body doesn’t operate that way. It’s a gradient. Bridging assumed a static risk, but thrombosis and bleeding are dynamic processes shaped by physiology, timing, and context.
DOACs don’t eliminate risk-they make it predictable. And predictability is the true enemy of unnecessary intervention.
Sam Mathew Cheriyan
22 December, 2025 . 00:29 AM
lol so now the government says bridging is bad but they still charge you $500 for doacs? and you think that’s fair? what if i can’t afford it? what if i’m from a poor family? they just want us to die on warfarin so they can sell us pills?
also… who says the BRIDGE trial wasn’t rigged? i heard the funding came from Pfizer. 😏