Agranulocytosis Risk Assessment Tool
Check Your Risk Level
This tool helps identify potential risk factors for medication-induced agranulocytosis based on the article's guidance. It is not a medical diagnosis - always consult your healthcare provider for clinical decisions.
When you take a new medication, you expect relief - not a life-threatening drop in your white blood cells. But for some people, common drugs can trigger agranulocytosis, a condition where neutrophils - the body’s first line of defense against infection - vanish almost overnight. Without enough of these cells, even a mild sore throat can turn into sepsis within hours. This isn’t rare. Up to 70% of all agranulocytosis cases are caused by medications, and without fast action, death rates can hit 20%.
What Exactly Is Agranulocytosis?
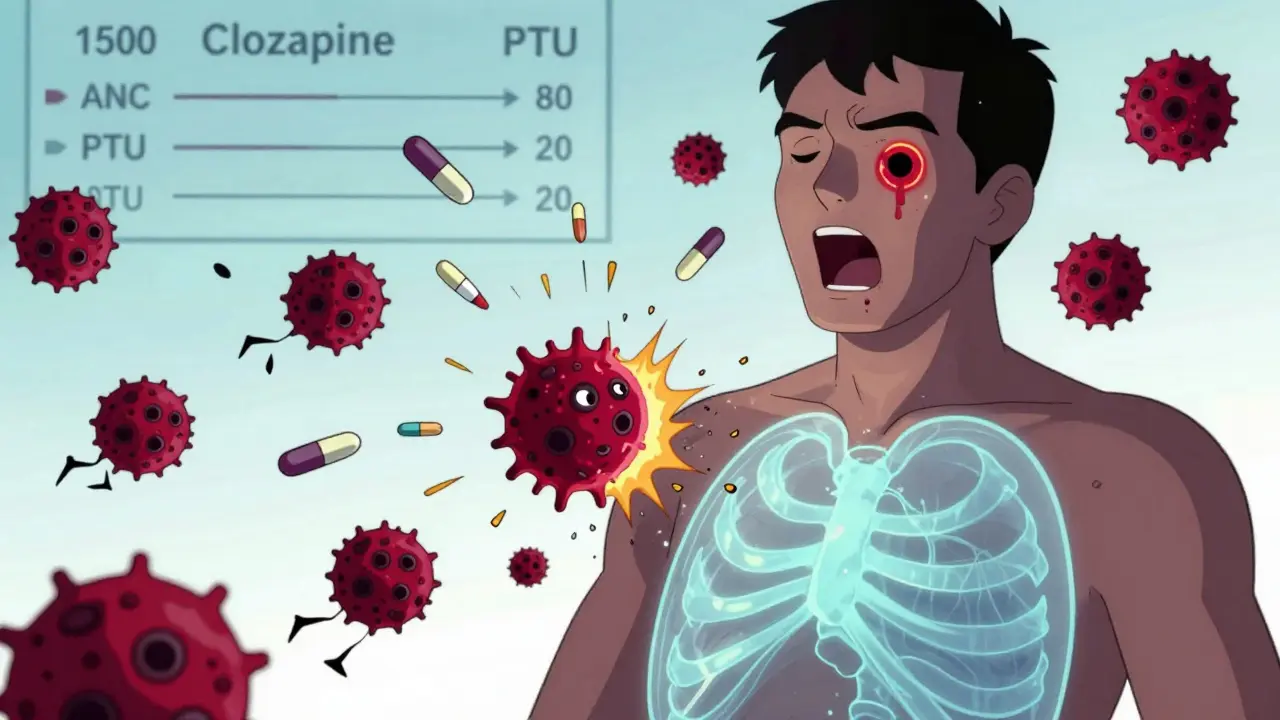
Agranulocytosis isn’t just low white blood cells. It’s when your absolute neutrophil count (ANC) drops below 100 per microliter of blood. For context, a normal ANC is between 1,500 and 7,000. When it falls below 100, your body can’t fight off bacteria or fungi. You might feel fine one day, then wake up with a fever, mouth ulcers, or a swollen throat - and crash within 24 hours.This isn’t a guess. It’s a medical emergency. The diagnosis requires two blood tests showing ANC under 100, plus a bone marrow exam confirming the absence of neutrophil precursors. Many patients are misdiagnosed at first. A 2022 survey found 63% of people had their early symptoms - fever, sore throat, fatigue - written off as a cold or flu. By the time they saw a specialist, their infection was already spreading.
Which Medications Are Most Likely to Cause It?
Over 200 drugs have been linked to agranulocytosis, but a few stand out because of how often they cause it and how serious the outcome can be.- Clozapine - Used for treatment-resistant schizophrenia, it carries the highest risk: about 0.8% of users develop agranulocytosis. That’s 8 in every 1,000 people. Because of this, the FDA requires weekly blood tests for the first 6 months of treatment, then every two weeks, then monthly. Even with this, 25% of cases happen in people who followed the rules.
- Propylthiouracil (PTU) - A drug for overactive thyroid. Its risk is 0.36 per 1,000 patient-years. Methimazole, another thyroid drug, is safer - only half the risk. Still, any patient on PTU needs monthly blood counts for at least the first 6 months.
- Trimethoprim-sulfamethoxazole - A common antibiotic for urinary tract and lung infections. People taking it are nearly 16 times more likely to develop agranulocytosis than those on other antibiotics.
- Dipyrone (metamizole) - Used for pain and fever in many countries (though banned in the U.S. and UK). It causes agranulocytosis in about 1.2 per 10,000 users.
- Some antipsychotics, anticonvulsants, and chemotherapy drugs - Also carry risk, though lower than clozapine or PTU.
Not all drugs are equal. Ibuprofen? Very low risk. Amoxicillin? Almost no link. The key is knowing which ones are dangerous - and who’s most at risk.
How Does a Drug Destroy Your Neutrophils?
There are two main ways drugs cause this:- Immune-mediated destruction (60% of cases) - The drug tricks your immune system into seeing your own neutrophils as invaders. Antibodies form, latch onto the cells, and destroy them. This can happen suddenly - sometimes within days of starting the drug.
- Bone marrow suppression (40% of cases) - The drug poisons the stem cells in your bone marrow that make neutrophils. This is slower. It often takes weeks or months before counts drop low enough to cause trouble.
With clozapine, it’s mostly immune-mediated. With chemotherapy, it’s usually bone marrow damage. That’s why timing matters. If you get sick right after starting a drug, it’s likely immune-driven. If symptoms appear after months, it’s probably the marrow being slowly poisoned.

Why Is Monitoring So Critical?
The good news? Agranulocytosis is preventable - if you catch it early.Studies show that when doctors stop the drug as soon as ANC falls below 500, and start antibiotics right away, death rates drop from 20% to under 5%. But that only works if someone is checking the numbers.
For clozapine, the rules are strict: weekly blood tests for the first 6 months. But a 2020 study found only 68% of U.S. doctors followed this. In rural areas, patients might drive 2 hours just to get a blood draw. Some skip it. Others wait until they feel sick - by then, it’s too late.
Now, there’s a new tool: point-of-care devices like the Hemocue WBC DIFF. This handheld machine gives a full white blood cell count in under 5 minutes. In a 2022 trial, using it increased monitoring adherence by over 30%. It’s not perfect - it doesn’t replace a full CBC - but it’s a game-changer for people without easy access to labs.
What Should You Do If You’re on a High-Risk Drug?
If you’re taking clozapine, PTU, or another high-risk medication, here’s what you need to do:- Know your baseline. Get an ANC test before starting the drug. Know what normal looks like for you.
- Stick to the schedule. Don’t skip blood tests. Even if you feel fine.
- Recognize the red flags. Fever over 38.3°C (101°F), sore throat, mouth sores, chills, or extreme fatigue - especially if you’ve been on the drug for weeks or months. These aren’t just “a cold.” Call your doctor immediately.
- Don’t wait for symptoms. If your ANC drops below 1,000 (even if you feel okay), your doctor should consider stopping the drug. New European guidelines now recommend acting at this level, not waiting until it hits 500.
- Ask about genetic testing. A new FDA-approved test (HLA-DQB1*05:02) can identify people with a 14-fold higher risk of clozapine-induced agranulocytosis. If you’re starting clozapine, ask if this test is available.
What Happens After Diagnosis?
Once agranulocytosis is confirmed, three things happen immediately:- The drug is stopped. No exceptions. Recovery starts the moment the trigger is removed.
- Antibiotics are started. You’re at high risk for bacterial and fungal infections. The Infectious Diseases Society of America recommends broad-spectrum antibiotics covering Pseudomonas - often drugs like piperacillin-tazobactam or meropenem. Delaying antibiotics increases death risk by 3x.
- Isolation and support. You may need to stay in a sterile environment. No flowers, no visitors with colds, no raw food. Your body can’t fight anything.
Recovery usually takes 1 to 3 weeks. Neutrophils bounce back once the drug is gone. But if you wait too long, you could lose your spleen, your lungs, or your life.

Why Are Some People Still Dying From This?
The problem isn’t the science. We know how to prevent this. The problem is access and awareness.Only 32% of low- and middle-income countries have formal monitoring programs. In rural Australia, patients might wait 5 days for a blood test. In the U.S., a 2023 CDC report found rural patients die from this condition 2.3 times more often than city dwellers.
Doctors miss it too. A survey of 347 patients found 73% blamed “lack of awareness among primary care providers.” Nurses don’t always know to ask about medications. Pharmacists don’t always flag the risks.
And patients? They’re not told. Many don’t know what neutrophils are. They don’t realize a sore throat on clozapine could kill them.
What’s Changing in 2025?
The field is moving fast:- AI alerts in EHRs - Hospitals are testing systems that automatically flag patients whose ANC is dropping, even if the doctor didn’t order a test. One trial cut missed cases by 47%.
- Genetic screening - By 2028, 40% of high-risk drugs may require genetic testing before prescription. If you carry HLA-DQB1*05:02, you won’t get clozapine unless you’re willing to accept higher risk.
- Centralized monitoring - The EU now requires pharmacies to report all prescriptions for high-risk drugs to national registries. If a patient misses a blood test, the system alerts their doctor.
These aren’t futuristic ideas. They’re already in use in Germany, Sweden, and parts of Australia. The question is: will they reach the people who need them most?
Final Thought: It’s Not About Fear - It’s About Awareness
You shouldn’t avoid life-saving medications because of rare side effects. Clozapine can restore someone’s ability to live normally when nothing else works. PTU can stop a thyroid storm. But you need to know the risks - and how to manage them.If you’re on one of these drugs, ask your doctor: “What’s my ANC? When’s my next test? What symptoms mean I need to come in right away?” Write them down. Set phone reminders. Tell a family member what to watch for.
Agranulocytosis is rare - but deadly. And it’s almost always preventable.





Cara C
21 December, 2025 . 21:22 PM
My aunt was on clozapine for years and never had an issue, but she got her blood drawn religiously. She’d set phone alarms for her labs like they were dentist appointments. If you’re on one of these meds, treat monitoring like brushing your teeth - not optional.
mukesh matav
22 December, 2025 . 08:58 AM
India doesn't even have consistent access to basic CBCs in rural clinics. How are we supposed to monitor for something this rare when the nearest lab is 80km away and the power’s out again? This feels like a rich-country luxury.
Peggy Adams
24 December, 2025 . 03:03 AM
So let me get this straight - big pharma knows these drugs can kill you, but they still push them because people will take them? And now they want us to pay for point-of-care machines? I’m just saying… what if the real cure is just not taking the damn pills in the first place?
Sarah Williams
25 December, 2025 . 23:40 PM
My cousin died from this after being told it was ‘just the flu.’ Don’t wait until you’re in the ER. If you’re on clozapine or PTU and feel off - even a little - get tested. Seriously. Your life is worth more than your fear of needles.
Jay lawch
27 December, 2025 . 08:46 AM
The real tragedy isn’t the drug - it’s the system that reduces human beings to lab numbers. We’ve turned healing into a spreadsheet. Neutrophils are not KPIs. A man’s life is not a risk percentage. The pharmaceutical-industrial complex profits from your fear and your compliance. They sell you hope, then charge you for the safety net. And when you fall? They say ‘we warned you.’ But who warned you about the warning? Who taught you to read the fine print in a language written by people who never had to live it?
Christina Weber
28 December, 2025 . 11:06 AM
There is a grammatical error in the post: ‘You might feel fine one day, then wake up with a fever, mouth ulcers, or a swollen throat - and crash within 24 hours.’ The em dash should be an em dash, not a hyphen. Also, ‘ANC under 100’ should be ‘ANC below 100’ - ‘under’ is imprecise in medical contexts. These details matter.
Dan Adkins
29 December, 2025 . 04:17 AM
It is a matter of grave concern that the Western medical paradigm continues to prioritize pharmacological intervention over holistic alternatives. In Nigeria, we have traditionally relied on herbal immunomodulators and spiritual cleansing to restore balance. The reduction of human physiology to neutrophil counts is not only reductive - it is a form of epistemic violence. Why are we not researching traditional remedies for immune support instead of reinforcing dependency on toxic synthetics?
Grace Rehman
30 December, 2025 . 04:54 AM
So we’re supposed to be grateful that AI is now going to nag us about our blood counts? Cool. Next they’ll beep when we forget to breathe. At least back in the day, you just had to trust your body - now we need a subscription to a wellness app just to not die from a pill
Siobhan K.
31 December, 2025 . 16:08 PM
I’m a pharmacist in Dublin - we’ve been using the EU registry system since 2023. If a patient misses a blood test, their pharmacy gets flagged, and their GP gets an automated alert. It’s not perfect, but it’s cut our missed cases by over half. The tech exists. The will is the problem.
Brian Furnell
2 January, 2026 . 09:41 AM
It’s critical to distinguish between immune-mediated and myelotoxic mechanisms - the former presents with rapid-onset neutropenia (often within 7–14 days of exposure) and is HLA-associated, while the latter is dose- and duration-dependent, with progressive marrow suppression detectable via serial differential counts. This distinction informs not only diagnostic urgency but also prognostic stratification and rechallenge risk profiles.
Southern NH Pagan Pride
3 January, 2026 . 15:09 PM
They say it's the drugs... but what if it's the chemicals they put in the water? Or the 5G towers? I know someone who got sick after starting PTU - and guess what? She started using a new phone right before. Coincidence? I think not. They don't want you to know the real cause
Orlando Marquez Jr
4 January, 2026 . 15:19 PM
While the clinical data presented is both robust and compelling, it is imperative to acknowledge the sociopolitical disparities in healthcare access that render these monitoring protocols inequitable. The notion of point-of-care diagnostics assumes infrastructural parity that does not exist across the global health landscape. A truly ethical approach must precede technological solutions.
Jackie Be
5 January, 2026 . 21:58 PM
My mom almost died from this and no one told her what to look for. I cried for weeks. If you’re on one of these meds - please, please, please don’t ignore a fever. I’m begging you. I’m not even joking. It’s not a cold. It’s a death sentence waiting to happen
John Hay
6 January, 2026 . 21:34 PM
My brother’s on clozapine. He’s alive because he gets his blood drawn every week like clockwork. I don’t care if it’s a pain - you do it. You set the reminder. You drive the distance. You do it because your life is worth more than your laziness.