The pandemic didn’t just change how we lived-it changed what medicines we could get, and for some, what drugs they could find at all. In early 2020, hospitals ran out of key drugs like sedatives and antibiotics. At the same time, street drugs became deadlier as fentanyl crept into everything. Two crises unfolded side by side: one in pharmacies, one on the streets.
Pharmaceutical Shortages Hit Hard in Early 2020
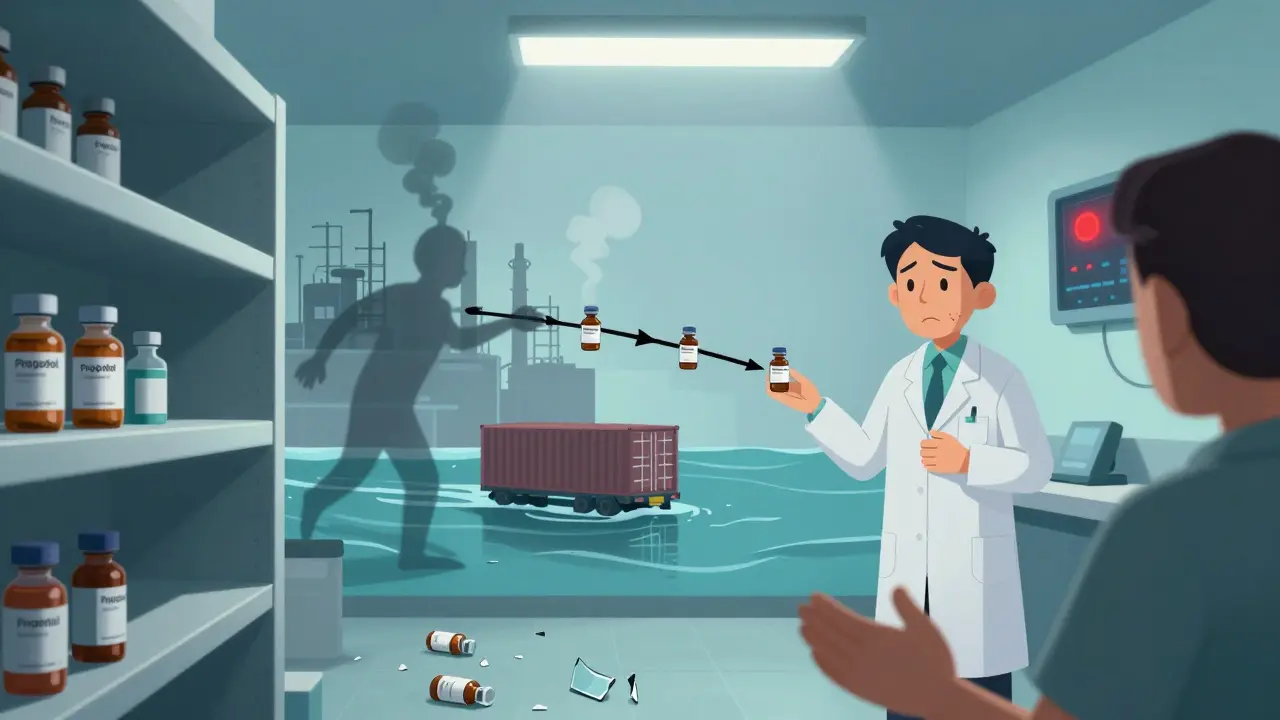
From February to April 2020, nearly 1 in 3 drug supply reports turned into actual shortages. That’s not a fluke-it was a system-wide breakdown. Critical care drugs like propofol, used to sedate COVID patients on ventilators, disappeared from hospital shelves. So did common medications like insulin, blood pressure pills, and antibiotics. People with chronic conditions started rationing. Some skipped doses. Others drove hours to find a pharmacy that still had stock.
A study in JAMA Network Open found that drugs with known supply chain issues were over four times more likely to have shortages during those first months. The problem wasn’t just demand. It was broken links in the chain: factories in China and India shut down, shipping slowed, and raw ingredients got stuck. Even simple things like glass vials or plastic caps became scarce. When one part of the system failed, everything else followed.
Why Shortages Dropped After May 2020
By May, things started to stabilize. Not because the pandemic ended, but because the FDA stepped in. They started calling manufacturers directly. They fast-tracked inspections. They pushed for transparency-asking companies to report problems before they turned into crises. Hospitals got better at managing inventory. Pharmacies switched to alternative brands. The shortage rate dropped from 34% of reports to under 10%.
But here’s the catch: the system didn’t fix itself. It was patched. The same vulnerabilities are still there. Most drugs still rely on overseas production. A single factory shutdown can ripple across the country. And without long-term policy changes, we’re just waiting for the next disruption.
The Illicit Market Got More Dangerous
While hospitals scrambled for medicine, the illegal drug market went dark-and then came back worse. Lockdowns cut off traditional supply routes. Dealers couldn’t move product the way they used to. So they turned to what was easy: fentanyl.
Fentanyl is cheap, powerful, and easy to ship in tiny amounts. It showed up in heroin, cocaine, meth, and even fake pills made to look like oxycodone or Xanax. Users didn’t know what they were taking. A Reddit user from June 2020 wrote: "I took the same dose I always did-and passed out. Turned out it was laced with fentanyl. My friend didn’t wake up."
Overdose deaths jumped. From May 2019 to April 2020, there were 77,007 deaths. The next year? 97,990. That’s a 27% increase in just 12 months. In states like West Virginia and Vermont, deaths rose over 50%. The CDC confirmed this wasn’t isolated-it was nationwide. The only states that saw drops were New Hampshire, New Jersey, and South Dakota.

Telehealth Helped Some, Left Others Behind
For people with opioid use disorder, the pandemic brought a strange mix of progress and loss. The government allowed doctors to prescribe buprenorphine over video calls. Take-home doses of methadone went from two weeks to four. For many, this was a lifeline. Especially in rural areas where clinics were hours away.
But not everyone could access it. Older adults struggled with apps. People without reliable internet got cut off. A 2020 survey found that 67% of addiction treatment centers had to cut services. Harm reduction programs-like needle exchanges and safe injection sites-lost 40% of their capacity in some cities. One Philadelphia program had to shut down its in-person services for weeks. They switched to drive-through naloxone distribution, but it wasn’t the same.
Behavioral support vanished. Group therapy, 12-step meetings, peer counseling-all gone. People in recovery lost their safety nets. And without those connections, relapse rates climbed.
Who Got Left Out?
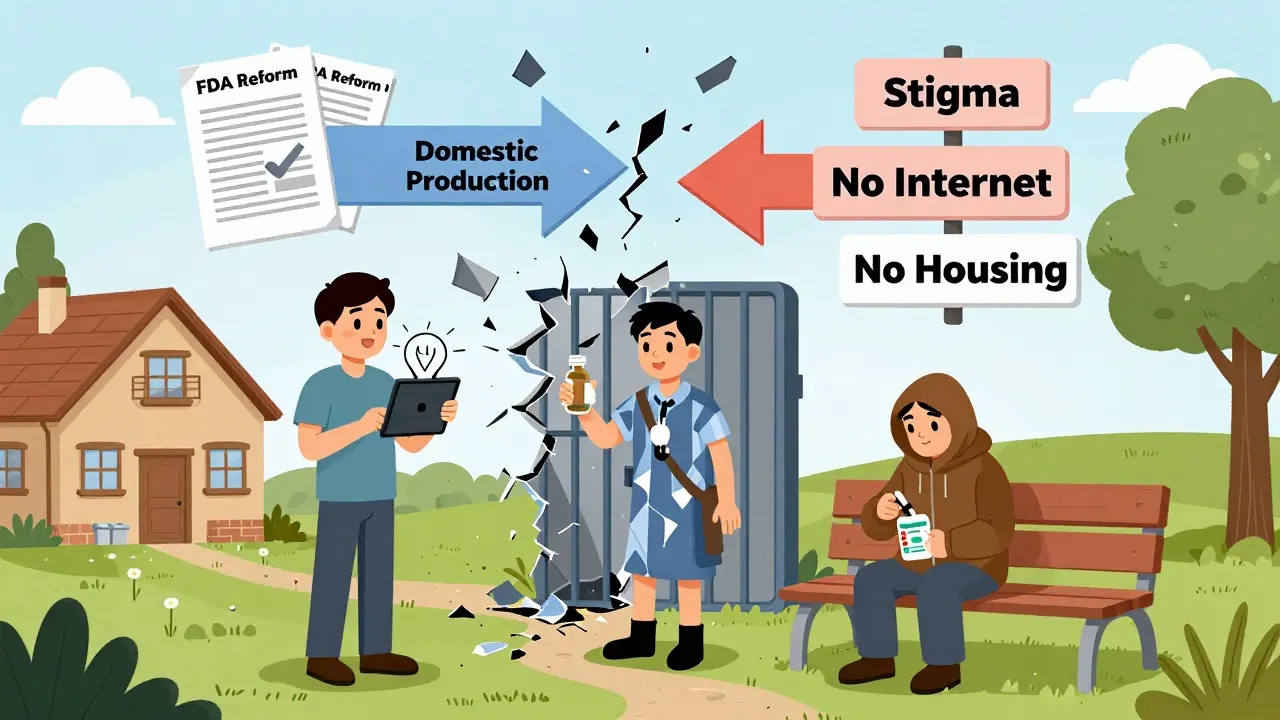
The pandemic didn’t affect everyone equally. People with stable housing, good insurance, and tech access got help. Those without? They were invisible.
Black, Indigenous, and Latino communities saw the steepest rises in overdose deaths. People experiencing homelessness couldn’t isolate. Incarcerated individuals lost access to medication-assisted treatment. Rural communities had fewer pharmacies and no telehealth infrastructure. And stigma kept many from seeking help. One user told researchers: "I didn’t call 911 when I overdosed. I was scared they’d arrest me."
The data is clear: the crisis wasn’t just about drugs. It was about poverty, racism, housing, and healthcare access-all made worse by lockdowns.
What’s Still Broken Today
Drug shortages are back to pre-pandemic levels. But that doesn’t mean they’re gone. They’re just quieter. The same factories still run on thin margins. The same global dependencies still exist. And without real reform, the next pandemic-or natural disaster, or war-will break it again.
Meanwhile, overdose deaths keep climbing. In 2022, over 107,000 people died from drug overdoses in the U.S. That’s higher than any year before. Fentanyl is still the main driver. Synthetic opioids now make up 70% of all overdose deaths.
Some progress is happening. The 2023 National Defense Authorization Act included new rules to track drug supply chains. The FDA is pushing for more domestic manufacturing. But these are baby steps. What we need is a system that doesn’t wait for crisis to act.
What Can Be Done?
Here’s what works:
- Build domestic supply chains for critical drugs-especially those used in emergencies.
- Require manufacturers to report supply risks before shortages happen, not after.
- Expand telehealth permanently for addiction treatment, with funding for internet access in rural areas.
- Decriminalize harm reduction-needle exchanges, fentanyl test strips, and safe consumption sites save lives.
- Invest in community-based care-not just clinics, but housing, jobs, and mental health support.
The pandemic showed us that drug availability isn’t just about production. It’s about justice. It’s about who gets care-and who gets left behind.




Tasha Lake
8 February, 2026 . 08:33 AM
So the systemic fragility in pharma supply chains is basically a perfect storm of just-in-time logistics + geopolitical fragility + zero buffer stock. We optimized for efficiency, not resilience. And now we’re paying for it with lives. Propofol shortages? That’s not an accident-it’s a design flaw. Same with insulin. We treat essential medicines like luxury goods instead of public infrastructure. And yet, no one’s talking about nationalizing critical production. Weird.
Karianne Jackson
8 February, 2026 . 19:59 PM
fentanyl in everything now 😭
Tom Forwood
10 February, 2026 . 14:17 PM
Man, I remember when my cousin in Ohio was trying to get her methadone dose during lockdown. She had to drive 90 miles because her clinic shut down. Meanwhile, the fentanyl pills she saw on Instagram were labeled "Oxy 30" but had enough punch to kill a horse. And nobody’s talking about how the DEA’s crackdown on pill mills just pushed everything to dark web vendors. It’s like we’re playing whack-a-mole with a damn nuclear bomb.
Also, telehealth was a lifesaver for some, but if you don’t have Wi-Fi or a smartphone that doesn’t freeze every 30 seconds? You’re SOL. We built a system that works great for people who already have privilege. Classic.
Chelsea Cook
11 February, 2026 . 21:12 PM
Oh wow, so the government ‘fixed’ shortages by begging manufacturers to tell them when they’re about to fail? That’s not a fix, that’s a pep talk. And we’re supposed to be impressed? 🤡
Meanwhile, fentanyl’s been the silent assassin of the opioid crisis, and we still haven’t made test strips legal in half the states. We’d rather jail someone for using than give them a $2 strip to stay alive. The moral logic here is… baffling.
Also, decriminalizing harm reduction isn’t ‘liberal fantasy’-it’s public health 101. Portugal did it. Now they have fewer overdoses and more people in treatment. We’re still stuck in 2002.
Andy Cortez
13 February, 2026 . 18:54 PM
you guys are overthinking this. the real problem? too many people think they deserve free medicine. like, no. you don’t. if you can’t afford insulin, maybe don’t have 3 kids and a vape collection? also, fentanyl? that’s just karma for doing drugs. if you wanna be a junkie, you take your chances. period. 🤷♂️
Jacob den Hollander
15 February, 2026 . 18:08 PM
Wow, this is so heartbreaking. I just want to say-thank you for writing this. It’s easy to forget that behind every statistic, there’s someone’s mom, brother, neighbor, coworker. I’ve seen people in recovery lose their support groups, their jobs, their housing-all because we didn’t prioritize connection. And that’s the real tragedy. Not just the drugs. Not just the shortages. But the isolation. We’re all in this together-even if we don’t realize it yet. Please, if you’re reading this and you’re struggling… you’re not alone. Reach out. Someone cares.
Also, I’m so glad someone mentioned telehealth. My aunt got her buprenorphine script via Zoom during the worst of it. She’s been clean for 18 months now. That’s a miracle. Let’s make that permanent. Please.
Randy Harkins
17 February, 2026 . 02:34 AM
This is so important. 💔 I’ve been in recovery for 5 years, and I’ve seen how fast everything can fall apart. When the clinics closed, I lost my group. I lost my routine. I almost relapsed. But I found an online peer group-just 12 people on Zoom every night. We didn’t have fancy therapy, but we had each other. That’s what saved me. Let’s fund those connections. Not just clinics. People. 🙏
Also, fentanyl test strips? I carry them everywhere. I got one from a friend at a gas station. It saved my life. Why are these still illegal? It’s insane.
Tori Thenazi
18 February, 2026 . 13:53 PM
Okay, but what if… this was all planned? 🤔
Think about it: the FDA suddenly ‘steps in’ right when the shortages peak? Coincidence? Or did they want to create chaos so they could ‘fix’ it with centralized control? And fentanyl? That’s not an accident-it’s a tool. Who profits from more overdoses? Pharma? The prison-industrial complex? The military-industrial complex? They all need more ‘crises’ to justify funding. This isn’t a breakdown-it’s a feature.
Also, why did the CDC only report drops in New Hampshire, New Jersey, and South Dakota? What’s special about those states? Are they secretly running a controlled experiment? I need answers.
Monica Warnick
20 February, 2026 . 13:36 PM
So basically, the system is broken. And we’re all just waiting for the next one. And the next. And the next. And we’re not doing anything. We just… accept it. That’s not resilience. That’s resignation.
Frank Baumann
21 February, 2026 . 00:55 AM
I’ve been working in hospital pharmacy for 22 years. I’ve seen this movie before. In 2008, we had a shortage of heparin. Then in 2011, it was vancomycin. In 2017, it was ampicillin. Every time, we’d panic for six months, then go back to business as usual. Why? Because no one’s willing to pay for redundancy. No one wants to spend $500M on a backup factory. But when someone dies because they couldn’t get a dose of propofol? Suddenly it’s a crisis. And then? Silence. Again. We’re not broken. We’re just numb. And the worst part? We know how to fix it. We just don’t want to. Because it’s cheaper to let people suffer than to fix the system. And that’s not just policy. That’s moral failure.
Chelsea Deflyss
21 February, 2026 . 17:29 PM
telehealth for addiction? lol. how many people even have a phone? or a room to themselves? or privacy? or a therapist who doesn’t judge? you think zooming in from a homeless shelter is gonna work? 🤡