Most people know they should eat more fiber-but few know which kind actually helps their gut. If you’re dealing with bloating, constipation, or unpredictable bowel movements, the difference between soluble and insoluble fiber isn’t just technical-it’s life-changing.
What’s the real difference between soluble and insoluble fiber?
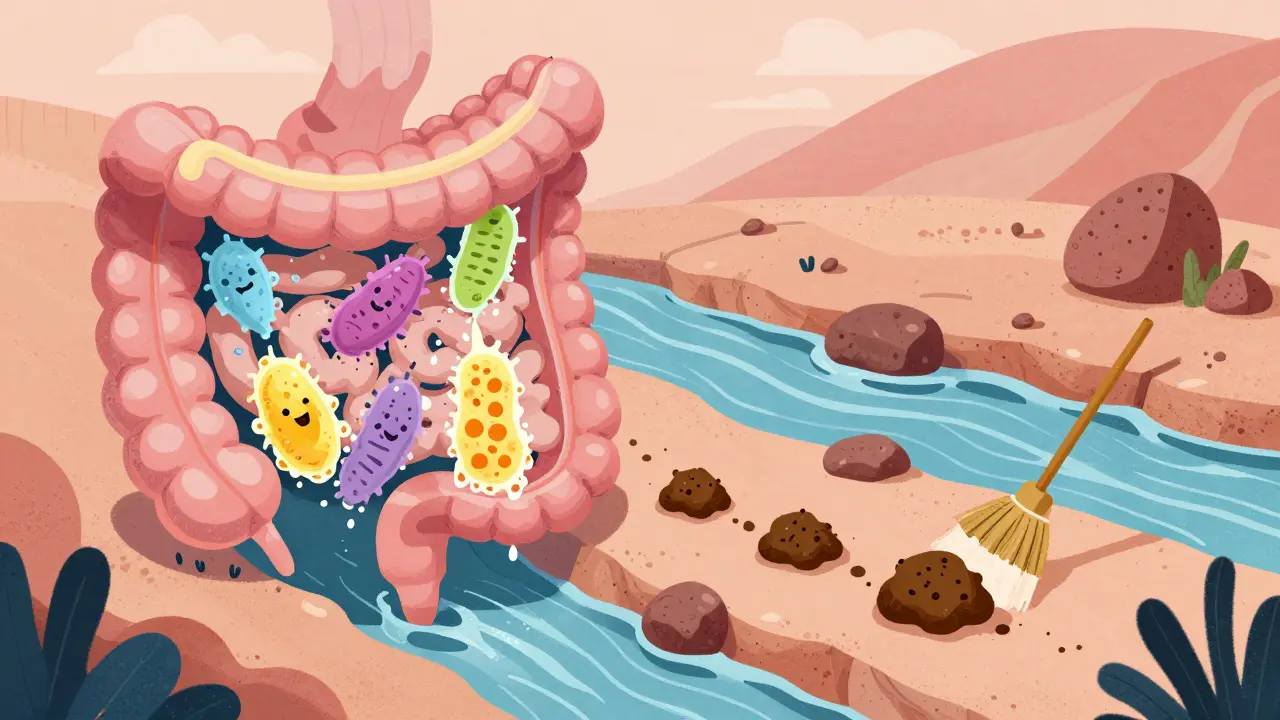
Soluble fiber dissolves in water. Think of it like a sponge soaking up liquid. When it hits your gut, it turns into a thick, gel-like substance that slows down digestion. This helps your body absorb nutrients more steadily, especially sugars. It also feeds the good bacteria in your colon, which then make short-chain fatty acids-tiny molecules that calm inflammation and strengthen your gut lining. Insoluble fiber doesn’t dissolve at all. It’s more like a broom. It moves through your digestive system mostly unchanged, picking up water along the way and adding bulk to your stool. That’s why it’s so good at keeping things moving. If you’re constipated, insoluble fiber is often the quick fix. The key? You need both. But not everyone needs them in the same amounts.Where do you find soluble fiber?
Soluble fiber shows up in foods that are soft, moist, or sticky when cooked. Oats are the classic example-just one bowl gives you about 2 grams. Beans and lentils are even better: a cup of cooked black beans delivers nearly 8 grams, mostly soluble. Chia seeds? A tablespoon soaked in water turns into a gel-5.6 grams of soluble fiber right there. Apples, carrots, and psyllium husk also pack a punch. These foods don’t just help your gut-they help your blood sugar. Studies show that eating 5-10 grams of soluble fiber daily can lower LDL (bad) cholesterol by 5-10%. For people with diabetes, it can cut post-meal blood sugar spikes by 15-20%. That’s because the gel slows how fast sugar enters your bloodstream. It’s also the fiber that helps with IBS. Many people with irritable bowel syndrome find relief with soluble fiber because it regulates stool consistency-whether you’re dealing with diarrhea or constipation. That’s why doctors often recommend psyllium husk or ground flaxseed for IBS. One Reddit thread from early 2023 showed that 68% of users with IBS saw improvement within two weeks of adding soluble fiber daily.Where do you find insoluble fiber?
Insoluble fiber comes from the tough parts of plants-the skins, husks, and bran. Whole-wheat flour has nearly 8 grams per 100 grams. Wheat bran? A staggering 12 grams. Nuts, seeds, and the skins of fruits like kiwi and apples are packed with it. Even popcorn counts-two cups give you about 3.5 grams. This fiber doesn’t get digested. Instead, it sweeps through your intestines, soaking up water and making stools softer and bulkier. That’s why it’s so effective for chronic constipation. Research shows it can reduce constipation risk by 30-50% by speeding up transit time by a day or two. But here’s the catch: if you have Crohn’s disease or ulcerative colitis during a flare-up, too much insoluble fiber can irritate your gut. The rough texture can scratch inflamed tissue. Experts recommend limiting insoluble fiber to 10-15 grams per day during flare-ups and only increasing it slowly as symptoms improve.
Why most people aren’t getting enough
The recommended daily intake is 25 grams for women and 38 grams for men under 50. But according to national health surveys, the average American eats just 15 grams. That’s less than half. Why? Because processed foods stripped out the fiber. White bread, pasta, and rice have almost none. Even many “healthy” breakfast cereals are low in fiber and high in sugar. If you’re eating mostly refined grains, you’re missing out. The problem isn’t just digestion. Low fiber intake is linked to higher rates of colon cancer, heart disease, and type 2 diabetes. The World Health Organization estimates that poor fiber intake contributes to over $195 billion in global healthcare costs each year.How to increase fiber without the bloating
Most people try to jump from 10 grams to 30 grams overnight-and end up bloated, gassy, and frustrated. That’s because your gut bacteria need time to adapt. The smart way: add 5 grams of fiber per week. Start with one extra serving of oats or beans. After a week, add a handful of almonds or a pear with the skin on. Keep going until you hit your target. And always drink water. For every 25 grams of fiber, aim for 1.5 to 2 liters of water daily. Without enough fluid, fiber turns into a brick in your intestines. That’s when constipation gets worse, not better.Whole foods over supplements
You can buy fiber supplements-psyllium, methylcellulose, inulin. They work. But they’re not better than food. Whole foods come with vitamins, minerals, antioxidants, and other plant compounds that work together. A chia seed isn’t just fiber-it’s omega-3s, magnesium, and lignans. A lentil isn’t just soluble fiber-it’s iron, folate, and slow-digesting protein. Studies show supplements can’t replicate the full benefits of whole foods. The gut microbiome responds differently to fiber that’s part of a natural food matrix. One 2024 review concluded that isolated fiber supplements don’t provide the same anti-inflammatory or metabolic benefits as fiber from fruits, vegetables, legumes, and whole grains.
What’s the ideal ratio?
There’s no magic number, but the Mediterranean Diet-a gold standard for gut and heart health-naturally hits a 3:1 ratio of insoluble to soluble fiber. That’s about 20-30 grams of insoluble and 10-15 grams of soluble per day. If you’re healthy and active, aim for that balance. If you have IBS, you might lean more toward soluble fiber. If you’re constipated and don’t have IBD, focus on adding insoluble fiber from bran, nuts, and whole grains. The goal isn’t to pick one over the other. It’s to get enough of both-through real food.What’s next for fiber science?
Scientists are now looking at personalized fiber plans. Companies like Viome and Zoe offer gut microbiome tests that show how your body responds to different types of fiber. Some people produce lots of butyrate from oats; others don’t. Some thrive on beans; others get bloated. In the next five years, doctors may start recommending specific fibers based on your unique gut bacteria-not just your age or gender. But for now, the advice is simple: eat more plants. More beans. More oats. More nuts. More skins. More vegetables. Your gut doesn’t need fancy supplements. It needs variety, consistency, and water.Can soluble fiber help with diarrhea?
Yes. Soluble fiber forms a gel that thickens loose stools and slows down digestion, which helps regulate bowel movements. People with IBS who experience frequent diarrhea often find relief by adding oats, chia seeds, or psyllium husk to their diet. It doesn’t stop diarrhea instantly, but consistent daily intake improves stool consistency over days to weeks.
Is insoluble fiber bad for IBD?
During flare-ups of Crohn’s disease or ulcerative colitis, insoluble fiber can irritate inflamed intestinal tissue. Foods like wheat bran, nuts, seeds, and raw vegetable skins may worsen cramping and diarrhea. Doctors typically recommend a low-residue diet during active flares, limiting insoluble fiber to 10-15 grams per day. Once symptoms improve, insoluble fiber can be gradually reintroduced to support long-term gut health.
Does fiber help with weight loss?
Yes, but indirectly. Soluble fiber slows digestion, which keeps you feeling full longer. It also triggers the release of gut hormones like GLP-1 and peptide YY, which signal fullness to your brain. Studies show this can reduce appetite by 20-25%. Fiber-rich foods are also usually lower in calories and require more chewing, which helps prevent overeating.
Can you get too much fiber?
Yes, but it’s rare from food alone. Too much fiber-especially from supplements-can cause bloating, gas, and even blockages if you’re not drinking enough water. The upper limit isn’t strictly defined, but most experts advise not exceeding 70 grams per day. The bigger risk is replacing nutrient-dense foods with fiber supplements or overloading on bran, which can interfere with mineral absorption.
What’s the best time to eat fiber?
There’s no perfect time. What matters is consistency. Spread your fiber intake across meals rather than loading it all into one. Eating fiber with meals helps slow sugar absorption and improves satiety. If you’re sensitive to gas, avoid high-fiber snacks right before bed. But overall, just make sure you’re getting enough throughout the day.
Do fiber supplements work as well as food?
They can help fill gaps, but they’re not better. Supplements like psyllium or inulin provide isolated fiber, but they miss out on the vitamins, minerals, antioxidants, and phytonutrients found in whole foods. Research shows the gut microbiome responds more positively to fiber from natural sources. For long-term gut health, food is always the first choice.



Hadi Santoso
16 December, 2025 . 11:40 AM
man i just started eating chia seeds last month and my bloating is way better, like overnight almost. no more afternoon stomach bombs. also i didn’t even know soluble fiber helped with blood sugar until this post. mind blown.
also psyllium husk is a game changer if you can get past the texture. mix it in yogurt or smoothies, don’t drink it straight lol.
Billy Poling
17 December, 2025 . 11:20 AM
While I appreciate the general overview presented herein, I must emphasize that the assertion regarding the efficacy of soluble fiber in managing IBS symptoms lacks sufficient citation of peer-reviewed longitudinal studies. The referenced Reddit thread, while anecdotal and potentially indicative of a trend, does not meet the threshold of empirical validation required for clinical recommendation. Furthermore, the conflation of dietary fiber with pharmaceutical-grade supplements may inadvertently promote a reductionist view of gastrointestinal physiology, which is inherently multifactorial and context-dependent.
Randolph Rickman
19 December, 2025 . 10:28 AM
Hey everyone, just wanted to say this post is 🔥. I used to have crazy constipation and switched to adding 1 tbsp ground flax + 1/2 cup black beans daily. Within 10 days, regular bowel movements - no laxatives needed. Also, drinking water with fiber? Non-negotiable. I used to skip it and then wonder why I felt like a brick factory inside.
Start slow. Be patient. Your gut isn’t a machine, it’s a garden. Water it, feed it, don’t dump fertilizer on it all at once.
Tiffany Machelski
20 December, 2025 . 00:09 AM
i never knew insoluble fiber could make flare ups worse. i’ve been eating raw kale every day like a health god. oops. gonna switch to steamed now. thanks for this.
Souhardya Paul
20 December, 2025 . 17:58 PM
One thing I’ve learned the hard way - fiber isn’t just about quantity, it’s about variety. I used to eat only oats and bran cereal, thought I was crushing it. Then I added lentils, apples with skin, chia, and almonds. My gut stopped acting like a drama queen. Also, psyllium isn’t magic - it’s just fiber with a fancy name. Same as flax, same as beans. Real food wins.
And yes, water. Always water. I used to drink coffee and think that counted. Nope.
Josias Ariel Mahlangu
21 December, 2025 . 04:47 AM
People these days think eating a few chia seeds makes them healthy. Back in my day, we ate whole grains, no supplements, no smoothies. We worked for our food. Now everyone wants a magic pill - or a gelatinous seed - to fix their laziness. Fiber isn’t a trend. It’s discipline.
anthony epps
22 December, 2025 . 14:33 PM
so soluble fiber = gel, insoluble = broom? that’s actually super easy to remember. i always got confused. thanks for making it simple.
Andrew Sychev
22 December, 2025 . 15:48 PM
I tried adding fiber and my gut turned into a warzone. Bloating for 3 weeks. Gas so bad my roommate moved out. I went to three doctors, two naturopaths, one psychic. Turns out I’m just not meant to be a ‘plant person.’ I miss my white bread. I miss my life.