When you’re managing high blood pressure, cholesterol, or heart disease, taking multiple pills every day becomes part of your routine. But what if you could cut that in half-or even more-without losing effectiveness? That’s the promise of cardiovascular combination generics: single pills that pack two or more heart medications into one. They’re not new, but they’re still underused. And for many people, they’re the smartest, simplest, and cheapest way to stick with treatment long-term.
Why Do These Combination Pills Even Exist?
It’s not just about convenience. Taking four separate pills a day is hard. Studies show that when patients have to manage multiple medications, adherence drops from around 60% to as low as 25%. That’s not laziness-it’s human. Life gets busy. Pills get lost. Side effects pile up. And when you forget one, you’re not just missing a dose-you’re increasing your risk of heart attack or stroke.
Combination generics solve this by putting drugs like a statin and a blood pressure pill into one tablet. The American Heart Association gives them a Class I recommendation-the strongest level-for improving adherence. Real-world data shows people taking single-pill combinations are 15-20% more likely to stick with their treatment than those on multiple separate pills.
The math is simple: fewer pills = fewer missed doses = fewer hospital visits.
What’s Actually in These Pills?
Not every combo is the same. The most common combinations you’ll find as generics include:
- Statins + ACE inhibitors: Atorvastatin + lisinopril
- Statins + ARBs: Rosuvastatin + losartan
- Beta-blockers + diuretics: Metoprolol + hydrochlorothiazide
- Statins + ezetimibe: Simvastatin + ezetimibe (generic version of Vytorin)
- Calcium channel blocker + diuretic: Amlodipine + hydrochlorothiazide
- Antiplatelet + statin: Aspirin + atorvastatin (available in some countries)
These combinations aren’t random. They’re based on clinical guidelines. For example, if you have high blood pressure and high cholesterol after a heart attack, your doctor might recommend a statin plus an ACE inhibitor or ARB. These drugs work together-statins lower LDL, ACE inhibitors reduce strain on the heart, and together they cut your risk of another event by up to 75%, according to research published in the European Heart Journal.
Some combos are newer. In 2022, the first generic version of sacubitril/valsartan (brand name Entresto) hit the market. This combo is used for heart failure and was once expensive and hard to access. Now, it’s affordable and widely available.
How Much Do They Save?
Let’s talk money. In 2017, Medicare data showed brand-name cardiovascular pills cost an average of $85.43 per fill. Generic versions? $15.67. That’s an 82% drop.
For combination generics, the savings are even bigger. A patient on three separate pills-say, atorvastatin, lisinopril, and hydrochlorothiazide-might pay $45 a month for generics. But if they switch to a single-pill combo containing all three, they could pay under $20. And if they were on brand-name versions? That same regimen could cost over $300 a month.
According to a 2020 Circulation study, if all eligible patients switched from brand-name to generic combinations, U.S. healthcare could save $1.3 billion annually. That’s not theoretical-it’s real money, right now.

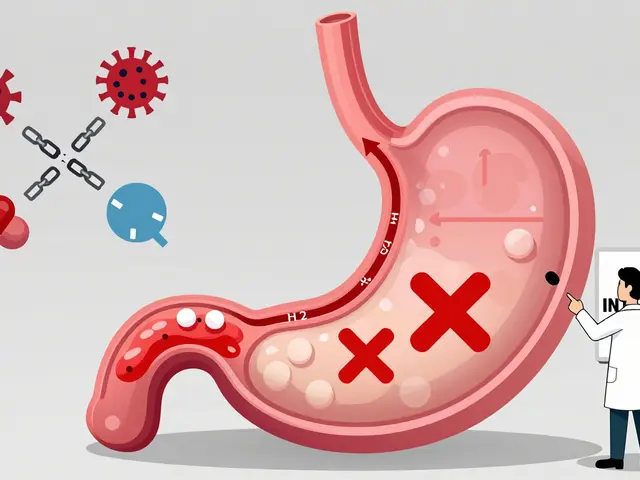
Are They as Safe and Effective as Brand Names?
This is the biggest concern patients have. “Will my generic heart pill work the same?”
The answer is yes-most of the time.
The FDA requires generic drugs to deliver 80-125% of the active ingredient compared to the brand name, within a 90% confidence interval. That’s a tight standard. A 2014 review of 61 clinical trials found no meaningful difference in safety or effectiveness between generic and brand-name cardiovascular drugs.
On Drugs.com, 78% of 1,245 patient reviews rated generic heart meds as “equally effective.” Only 12% reported minor side effect changes-usually things like dizziness or fatigue, which often resolve as the body adjusts.
There’s one exception: warfarin. Because it has a narrow therapeutic window (too little doesn’t prevent clots, too much causes bleeding), switching brands-even to a generic-can require closer monitoring. But for statins, ACE inhibitors, beta-blockers, and most other heart meds? No evidence of risk.
Some patients report feeling different after switching. That’s often not the drug-it’s the filler. Generic pills use different inactive ingredients (dyes, binders, coatings). For most people, it doesn’t matter. But if you have a rare sensitivity (say, to lactose or a specific dye), you might notice a change. Talk to your pharmacist if you feel off after switching.
What’s Missing? The “Polypill” Gap
Back in 2002, Dr. Salim Yusuf proposed the “polypill”-a single tablet with aspirin, a statin, a beta-blocker, and an ACE inhibitor. It could prevent 75% of cardiovascular events in high-risk patients.
Here’s the problem: that exact combo doesn’t exist as a single generic pill in the U.S.
Why? Regulatory hurdles. Drug companies don’t always invest in combos unless there’s a patent to protect. Since all the individual drugs are off-patent, no one has a financial incentive to bundle them into one pill and get it approved as a new product.
So while you can get statin + ACE inhibitor, or beta-blocker + diuretic, you can’t yet get all four in one tablet here. In India, the UK, and parts of Latin America, polypills are already in use. The World Heart Federation is pushing for them globally, especially in low-income countries where access to multiple meds is a barrier.
For now, in the U.S., you may need two pills: one for your cholesterol and blood pressure, another for your beta-blocker or aspirin. Still, that’s a big improvement over four.
What Are the Alternatives?
If a combination generic isn’t available for your exact needs, you have options:
- Stick with separate generics: This is still better than brand names. Amlodipine, atorvastatin, lisinopril, and metoprolol are all dirt cheap as generics.
- Ask about therapeutic substitution: Your doctor might be able to swap one drug for another that has a combo version. For example, if you’re on metoprolol tartrate (short-acting), switching to metoprolol succinate (long-acting) might allow you to use a combo pill.
- Use a pill organizer: If you’re stuck with multiple pills, a weekly pill box with alarms can help you stay on track. Some pharmacies offer pre-filled organizers for free.
- Check mail-order pharmacies: Many offer 90-day supplies of generics at lower prices. Some even include free pill organizers.
Don’t assume you have to take what your doctor first prescribed. Ask: “Is there a generic combo that covers what I need?”

Why Aren’t More Doctors Prescribing Them?
Surprisingly, only 45% of primary care doctors in the U.S. were familiar with all available generic combinations as of 2018. Why? Time. Training. Outdated formularies.
Doctors don’t always know which combos are covered by insurance or which ones are actually available. Pharmacists, on the other hand, are often ahead of the curve. In fact, 89% of pharmacists routinely explain to patients that generics are just as safe.
If your doctor says, “I don’t prescribe those,” ask: “Can you check if there’s a combo version for my meds?” Or better yet, ask your pharmacist. They can suggest alternatives and even contact your doctor on your behalf.
What Should You Do Next?
Here’s a simple action plan:
- Write down every heart medication you take-name, dose, frequency.
- Ask your pharmacist: “Are any of these available in a generic combination pill?”
- Bring that list to your doctor: “I’d like to reduce my pill burden. Are there combo options that fit my treatment?”
- Check your copay: If you’re paying more than $20/month for heart meds, you’re likely paying too much.
- Don’t panic if you switch: Minor side effects in the first week are normal. If they last longer, call your doctor.
Most people who switch to combination generics report feeling more in control. No more scrambling to remember which pill goes when. No more refill confusion. Just one pill. One routine. One less thing to worry about.
Frequently Asked Questions
Are cardiovascular combination generics safe?
Yes, for most people. The FDA requires generics to meet strict bioequivalence standards-80-125% of the brand’s active ingredient. A 2014 review of 61 clinical trials found no difference in safety or effectiveness between generic and brand-name cardiovascular drugs. The exception is warfarin, which needs careful monitoring during any switch.
Can I switch from brand-name to generic combination pills on my own?
No. Always talk to your doctor first. Even though generics are safe, your medication plan is personalized. Switching without guidance could affect your blood pressure, heart rate, or cholesterol control. Your doctor may need to adjust doses or monitor you briefly after the switch.
Why aren’t there more combo pills available?
Because drug companies have little financial incentive to create new combos when all the ingredients are off-patent. There’s no profit in bundling cheap generics. So while individual drugs are widely available as generics, multi-drug combos are limited. Some, like statin + ACE inhibitor, are common. Others, like the full polypill (aspirin + statin + beta-blocker + ACE inhibitor), aren’t approved in the U.S. yet.
Do combination generics cause more side effects?
Not usually. The active ingredients are identical to the brand versions. But inactive ingredients (fillers, dyes, coatings) can differ. A small number of patients report mild side effects like dizziness or fatigue after switching, often because their body is adjusting. If symptoms persist beyond a week, contact your doctor.
How do I know if my insurance covers a combination generic?
Call your pharmacy or check your plan’s formulary online. Most Medicare Part D and private insurers cover generic combinations at the lowest tier-often under $10 per month. If your current meds cost more than $20/month, ask your pharmacist to check for a cheaper combo alternative.


Paul Dixon
11 December, 2025 . 03:44 AM
I switched to a statin + BP combo last year and my life changed. No more pill organizer chaos, no more forgetting which one I took at lunch. Just one pill with breakfast. My doc was skeptical, but my numbers are better and my wallet is happier. Seriously, if you’re on three or more heart meds, ask your pharmacist about combos. It’s not magic-it’s just smart.
Aman deep
12 December, 2025 . 01:43 AM
bro in india we got the full polypill since 2018 like literally aspirin + atorva + metoprolol + lisinopril in one tab and its like 50 rupees a month 😭 my uncle who had a stent last year takes it and says he feels like a new man. why cant america just do this?? i get patents and stuff but like… people are dying from cost not disease. this is wild.
Sylvia Frenzel
12 December, 2025 . 23:29 PM
Generic heart pills? Sounds like another government-approved shortcut. My uncle took generics and ended up in the ER because his blood pressure crashed. I don’t trust these cheap knockoffs. If it’s your heart, don’t gamble with it. Brand names exist for a reason.
Doris Lee
13 December, 2025 . 07:34 AM
This is the kind of post that makes me feel hopeful. I used to dread my pillbox, now I just pop one tablet and feel like I’m actually doing something right. Don’t let fear stop you from asking your pharmacist-they’re the real heroes here. You’ve got this.
Stephanie Maillet
13 December, 2025 . 17:35 PM
It’s fascinating-this isn’t just about pharmacology; it’s about systemic inertia. We’ve optimized for profit over pragmatism. The polypill isn’t a scientific gap-it’s a policy failure. Why do we incentivize complexity when simplicity reduces mortality? The answer lies not in medicine, but in the architecture of capitalism. And yet… here we are, still trying to make the system work for people, not just shareholders.
john damon
14 December, 2025 . 11:39 AM
OMG YES 😭 I just switched to the amlodipine + HCTZ combo and I’m crying happy tears. No more 6 pills a day. Just one. And it’s $8 at CVS. My grandma used to say, "Less is more," and she was right. 🙌
Taylor Dressler
16 December, 2025 . 04:34 AM
Important clarification: The FDA’s 80–125% bioequivalence range applies to the rate and extent of absorption, not just peak concentration. For cardiovascular drugs, this is rigorously tested across multiple dosing regimens. A 2014 meta-analysis in JAMA Cardiology reviewed over 12,000 patients and found zero clinically significant differences in outcomes between generics and brands for statins, ACEIs, and beta-blockers. The exception remains warfarin due to its narrow therapeutic index. Always consult your provider before switching, but the data is overwhelmingly supportive.
Aidan Stacey
17 December, 2025 . 10:18 AM
My cardiologist didn’t even know about the new generic sacubitril/valsartan until I showed him the pharmacy receipt. $12 vs $400. He was stunned. Then he apologized. That’s the problem-doctors are drowning in info, but pharmacists? They’re the ones holding the map. Ask your pharmacist. Seriously. They know more than your doctor does about what’s actually available and affordable.