Anaphylaxis Recognition Tool
Assess Your Symptoms
This tool helps determine if symptoms indicate anaphylaxis based on the American Academy of Allergy, Asthma & Immunology criteria. It is not a substitute for medical advice.
What Anaphylaxis Really Looks Like
It happens fast. One moment, someone feels fine. The next, their throat closes, their skin breaks out in hives, and their blood pressure plummets. This isn’t just a bad rash or a panic attack. This is anaphylaxis - a sudden, full-body allergic reaction that can kill within minutes. And when it’s triggered by a medication, it’s often missed until it’s too late.
Medications cause about 1 in 6 anaphylaxis cases in hospitals and clinics. Antibiotics like penicillin are the biggest culprits, making up nearly 70% of drug-related reactions. But it’s not just antibiotics. NSAIDs like ibuprofen, monoclonal antibodies used in cancer and autoimmune treatments, and even IV contrast dyes can set off this deadly chain reaction. The problem? Many healthcare workers and patients don’t recognize the signs early enough.
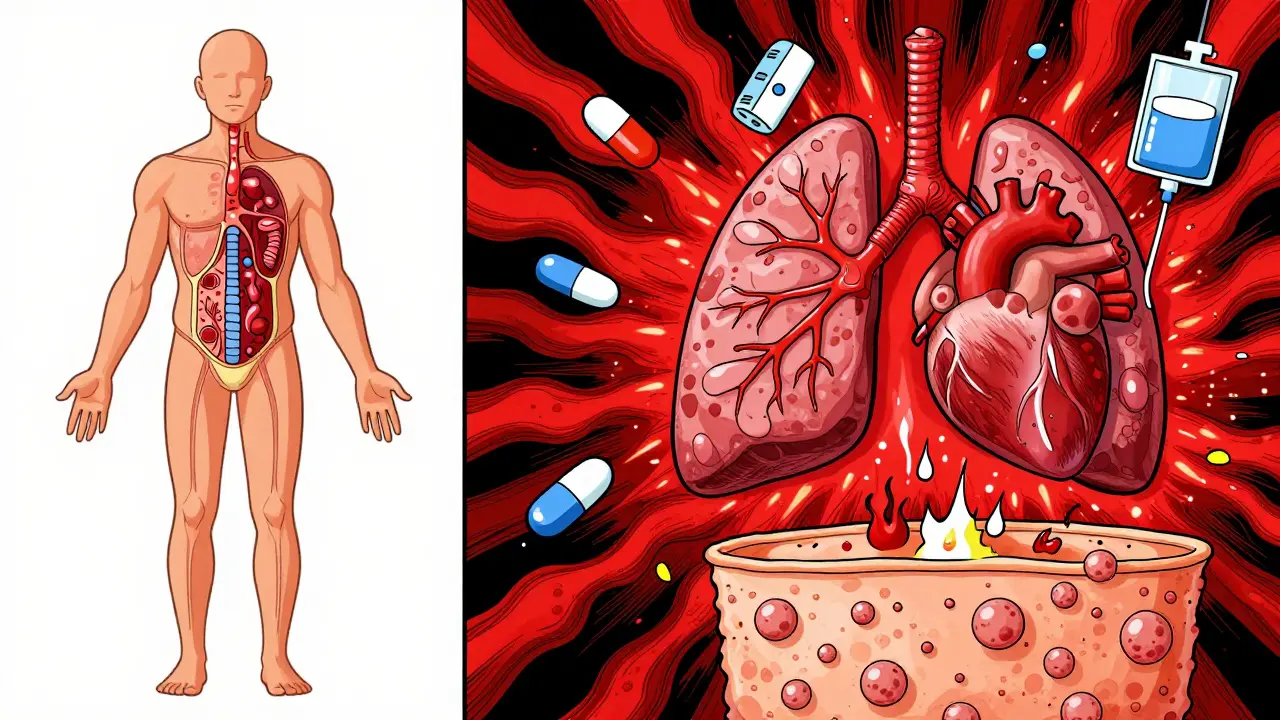
How Your Body Turns Against a Drug
Anaphylaxis isn’t a simple allergy. It’s a system-wide explosion. When your immune system mistakes a medication for a threat, it triggers mast cells and basophils to dump histamine, tryptase, and other chemicals into your bloodstream. These chemicals make blood vessels leak fluid, cause airways to tighten, and drop your blood pressure. It’s like your body suddenly declares war on something meant to help you.
The timing matters. With IV meds, symptoms can start in under 5 minutes. Oral meds might take up to 30 minutes. Delayed reactions can even show up 6 hours later. That’s why a patient who seems fine after a shot isn’t necessarily safe. You can’t wait for the classic signs - you have to act on the first warning.
The Three Signs That Mean It’s Anaphylaxis
The American Academy of Allergy, Asthma & Immunology (AAAAI) says anaphylaxis is likely if any one of these three things happens after taking a drug:
- Skin symptoms (hives, swelling, itching) plus trouble breathing or low blood pressure.
- Two or more systems affected - skin, lungs, heart, gut - after exposure to a likely trigger.
- Low blood pressure alone after being exposed to a known allergen.
That’s it. No need for a full list of symptoms. If you see one of these, treat it as anaphylaxis. Don’t wait for more signs. Don’t assume it’s something else.
Here’s what to watch for:
- Skin: Hives, flushing, swelling of lips, tongue, or throat.
- Breathing: Wheezing, shortness of breath, stridor (a high-pitched sound when breathing in), feeling like your throat is closing.
- Heart: Rapid pulse, dizziness, fainting, low blood pressure - this is the most dangerous sign.
- Stomach: Nausea, vomiting, cramps, diarrhea.
Here’s the key difference between medication-induced anaphylaxis and food-induced: drug reactions are more likely to hit the heart and lungs hard. About 58% of medication cases involve low blood pressure, compared to 39% with food. That’s why it’s deadlier - 1.8% of drug-induced cases end in death, versus 0.7% for food.
Why It’s Often Missed - and What Happens When It Is
Doctors and nurses don’t always see it coming. In a 2022 survey of over 1,200 clinicians, nearly 7 out of 10 admitted they’d misdiagnosed anaphylaxis at least once. Common mistakes:
- Calling it a vasovagal reaction (fainting) when someone goes pale and dizzy after an IV.
- Blaming it on anxiety or panic - especially if the patient is nervous about the shot.
- Thinking it’s sepsis because of fever or low blood pressure.
- Confusing red man syndrome (a reaction to rapid vancomycin infusion) with true anaphylaxis. Red man syndrome causes flushing and itching but doesn’t cause low blood pressure or breathing trouble.
And when it’s missed? The results are brutal. A 2023 review found that 78% of fatal anaphylaxis cases involved delayed or missed epinephrine. In over a third of those cases, epinephrine wasn’t given at all. That’s not a treatment failure - it’s a recognition failure.
Epinephrine: The Only Thing That Saves Lives
There’s only one drug that stops anaphylaxis in its tracks: epinephrine. Not antihistamines. Not steroids. Not oxygen. Epinephrine. It tightens blood vessels, opens airways, and stabilizes the heart. And it has to be given fast - within 5 to 15 minutes of symptom onset.
Studies show that if epinephrine is given after 30 minutes, the risk of death jumps by 300%. That’s not a typo. Every minute counts.
How to give it right:
- Use an auto-injector (EpiPen, Auvi-Q, etc.) or a syringe with 0.3-0.5 mg for adults.
- Inject into the outer thigh - through clothing if needed.
- Hold for 3 seconds to make sure the full dose goes in.
- Call 911 immediately, even if symptoms improve.
Don’t wait for a doctor. Don’t call the nurse. Give it yourself if you’re trained. If you’re with someone who’s reacting and they’re unconscious, give it anyway. The risk of giving it when it’s not needed is far lower than the risk of not giving it.
What Comes After the Emergency
Surviving anaphylaxis doesn’t mean you’re done. Many patients leave the hospital without a plan. A 2023 survey by Allergy & Asthma Network found that over half of people who had a drug-induced reaction never got an epinephrine auto-injector prescribed to them. That’s a massive gap.
After the crisis, you need:
- A written emergency action plan.
- Referral to an allergist for testing - skin or blood tests can confirm the trigger.
- Medical alert jewelry or a digital alert in your phone.
- Clear documentation in your medical records - not just "allergy to penicillin," but the exact drug, dose, route, and symptoms.
Electronic health records are still failing here. A 2023 study found that over 60% of anaphylaxis cases linked to medication errors happened because the allergy wasn’t properly recorded in the system. If your chart says "penicillin allergy," but it’s not detailed, a doctor might still give you amoxicillin - and you might not survive.

How Hospitals Are Getting Better
Some places are making real progress. Johns Hopkins Hospital cut hospital anaphylaxis cases by 47% just by improving how allergies are documented and flagged in their system. The Cleveland Clinic reduced the time to give epinephrine from over 12 minutes to under 5 minutes by training staff on a simple 5-minute recognition protocol.
Simulation training works. At one hospital, after staff practiced anaphylaxis scenarios, epinephrine use jumped from 48% to 90% in real cases. That’s not magic - it’s practice.
New tools are coming too. In June 2023, the FDA approved the first rapid test for penicillin allergy - a finger-prick test that gives results in 15 minutes. And AI tools are being tested to predict who’s at risk before a drug is even given, using data from past reactions, genetics, and medical history.
What You Can Do Right Now
If you’ve ever had a reaction to a drug - even a mild one - document it. Write down:
- What drug you took
- How much
- How it was given (pill, shot, IV)
- Exactly what happened (hives? throat tightness? passing out?)
- When it started
Share that with every doctor, dentist, and pharmacist. Don’t say "I’m allergic to antibiotics." Say "I broke out in hives and had trouble breathing after taking amoxicillin in 2022."
If you’re a caregiver, know the signs. If someone suddenly looks sick after a new medication, don’t wait. Check their breathing. Look for swelling. Feel for a weak pulse. If in doubt - give epinephrine. Call 911. Then call again if they don’t improve.
What’s Changing in 2025
Starting January 1, 2024, every hospital and clinic in the U.S. that’s accredited by The Joint Commission must have a written anaphylaxis recognition and response protocol. That means staff training, clear signage, epinephrine kits in every treatment room, and mandatory documentation.
The WHO is pushing for a global goal: cut fatal medication-induced anaphylaxis by 50% by 2030. That’s ambitious - but possible. The biggest barrier isn’t science. It’s awareness. Too many people still think anaphylaxis looks like a cartoon version of swelling and hives. It doesn’t. It looks like someone who’s suddenly too quiet, too pale, too still. That’s the moment you act.





Miriam Piro
27 December, 2025 . 15:49 PM
So let me get this straight... the pharmaceutical industry *wants* us to panic over meds so they can sell us epinephrine pens and push more $$$ tests? 🤔 They’ve been hiding the truth since the 50s. Did you know the FDA approved penicillin *without* proper long-term trials? And now they’re pushing AI to predict reactions? That’s just a fancy way to track your DNA and sell you insurance. Wake up. This isn’t medicine-it’s control. #BigPharmaLies 🤫💉
dean du plessis
28 December, 2025 . 02:34 AM
I’ve seen this happen in a rural clinic in Cape Town. Nurse gave a kid amoxicillin, he went quiet, skin turned white, no wheezing just... still. She didn’t know what to do. Took 10 minutes to get epinephrine. Kid survived. But we lost three others last year. People need to know this isn’t theoretical. It’s happening right now.
Kylie Robson
28 December, 2025 . 17:40 PM
The pathophysiology here is textbook type I hypersensitivity mediated by IgE cross-linking on mast cell FcεRI receptors, triggering degranulation and release of preformed mediators like histamine, tryptase, and heparin, plus newly synthesized leukotrienes and prostaglandins. The hemodynamic collapse is due to systemic vasodilation and increased vascular permeability-classic distributive shock. Epinephrine works via alpha-1 adrenergic agonism to reverse vasodilation and beta-2 effects to bronchodilate. Everything else is adjunctive. Stop treating symptoms. Treat the mediator cascade.
Caitlin Foster
29 December, 2025 . 22:40 PM
Okay but WHY do we still have hospitals without epinephrine in EVERY room?? 🤯 Like are we just waiting for someone to die before we fix this?? I had a cousin almost die because the nurse ‘didn’t think it was serious’ and went to get a doctor. A DOCTOR??!?!?!! Epinephrine is the FIRST RESPONDER, not the guest speaker at the end of the show!! #EpinephrineNow #StopWaiting
Todd Scott
30 December, 2025 . 03:47 AM
In Nigeria, we don’t have EpiPens in most clinics. But we’ve adapted. We train community health workers to recognize the silent signs-the pallor, the stillness, the lack of response. We use intramuscular epinephrine from vials with syringes. We teach families to hold the thigh, count to three, and call for help. It’s not perfect. But it saves lives. Culture matters. Access matters. And we’re building it from the ground up.
Andrew Gurung
30 December, 2025 . 06:13 AM
Ugh. Another ‘educational’ post that pretends this is just about ‘awareness.’ 😒 The real issue? The medical establishment has been *complicit*. They don’t want you to know that most ‘allergies’ are misdiagnosed. They profit from lifelong fear, unnecessary avoidance, and repeat visits. They’d rather you carry a pen than fix the system. And don’t even get me started on the FDA’s cozy relationship with Big Pharma. This isn’t saving lives-it’s maintaining the illusion of safety. 🙄💉
James Bowers
1 January, 2026 . 03:57 AM
It is imperative to underscore that the administration of epinephrine in the context of anaphylactic shock constitutes the sole therapeutic intervention with demonstrated mortality-reducing efficacy. All other modalities-including antihistamines, corticosteroids, and oxygen supplementation-are palliative at best and should never delay definitive treatment. The failure to administer epinephrine within the first fifteen minutes constitutes a clinically significant deviation from the standard of care, and in many jurisdictions, may constitute negligence.
Janice Holmes
1 January, 2026 . 11:40 AM
I WAS THE ONE WHO ALMOST DIED. 🫠 I got IV vancomycin. Started itching. Thought it was ‘red man syndrome.’ Didn’t tell anyone. Thought I was fine. Then my chest felt like a vise. I couldn’t breathe. My legs gave out. I was on the floor. They didn’t give epinephrine for 18 minutes. I woke up in ICU. They told me I was ‘lucky.’ Lucky? I had to relearn how to breathe. I have PTSD from that IV pole. I don’t trust hospitals anymore. And now they want me to ‘document it’? I can’t even say the word ‘antibiotic’ without my hands shaking. This isn’t a blog post. This is my life.
Jane Lucas
2 January, 2026 . 05:29 AM
my sister had this happen after a flu shot. just looked tired. then her lips swelled. we panicked. called 911. they gave her benadryl first. took 15 mins to get epinephrine. she’s fine now. but why did they wait? why? i dont get it.
Elizabeth Alvarez
3 January, 2026 . 10:59 AM
You think this is about medicine? Nah. This is about the CDC and WHO pushing mandatory vaccination tracking. They need you to fear every shot so you’ll sign up for their digital health passports. They’re using anaphylaxis as a scare tactic to control your medical choices. Penicillin? No. It’s the RFID chips in the syringes. You think the ‘rapid test’ is for allergies? It’s for biometric logging. They already know who you are. They’re just waiting for you to panic so they can lock you down. Wake up. This isn’t science. It’s surveillance.
Paula Alencar
4 January, 2026 . 23:25 PM
As a nurse educator in a Level I trauma center, I have witnessed the devastating consequences of delayed epinephrine administration on multiple occasions. The implementation of standardized anaphylaxis protocols, including mandatory simulation-based training for all clinical staff, has demonstrably improved outcomes. However, the most critical component remains cultural: we must foster an environment in which any clinician, regardless of rank, feels empowered to initiate life-saving intervention without awaiting explicit authorization. Patient safety is not a hierarchy-it is a collective responsibility.
Nikki Thames
5 January, 2026 . 15:39 PM
I’m sorry, but if you’re relying on a random Reddit post to understand anaphylaxis, you’re already one step away from tragedy. This isn’t a ‘life hack.’ It’s a medical emergency that requires formal education, certification, and clinical oversight. You don’t ‘learn’ this from a blog. You learn it in residency. You learn it in simulation labs. You learn it by watching someone die because someone else thought it was ‘just anxiety.’ If you’re not a trained professional, your opinion on this topic is not just irrelevant-it’s dangerous.
Chris Garcia
7 January, 2026 . 02:35 AM
In my village in Lagos, we say: 'When the body speaks in silence, the mind must listen.' This post speaks truth-but it speaks only to those who already have access. What of the mother who walks five kilometers to a clinic with no electricity, no epinephrine, no trained staff? We need not just protocols-but justice. Not just training-but equity. The science is clear. The will? That is the real allergy. And it is killing us.