When it comes to catching lung cancer early, low-dose CT screening isn’t just a nice-to-have-it’s life-saving for the right people. But knowing whether you qualify and what the results actually mean can be confusing. Many assume if they’ve smoked, they’re automatically eligible. Others worry the scan will find something harmless and send them down a rabbit hole of tests. The truth? It’s not that simple. But with the right info, you can make a clear, confident decision.
Who Is Actually Eligible for Low-Dose CT Screening?
The rules for who gets screened changed in 2021, and they’re not the same everywhere. The U.S. Preventive Services Task Force (USPSTF) now recommends annual low-dose CT scans for adults aged 50 to 80 who have smoked at least 20 pack-years-and who still smoke or quit within the last 15 years.
What’s a pack-year? Multiply the number of packs you smoked per day by the number of years you smoked. So, one pack a day for 20 years equals 20 pack-years. Two packs a day for 10 years? Also 20. It doesn’t matter if you smoked cigarettes, cigars, or pipes-what counts is total exposure.
But here’s where it gets messy. Medicare covers screening for people 50 to 77. The American Cancer Society says 50 to 80, with no upper limit on how long ago you quit. The National Comprehensive Cancer Network goes even further-up to age 85, and they include people with other risk factors like family history of lung cancer, exposure to asbestos or radon, or a history of pulmonary fibrosis.
That means you could be eligible under one guideline but not another. The bottom line? If you’re between 50 and 80 and have a 20-pack-year history, talk to your doctor. Even if you quit more than 15 years ago, your risk doesn’t drop to zero. Studies show over a third of lung cancers happen in people who quit more than 15 years ago. That’s why some experts argue the quit-time cutoff is outdated.
What Does a Low-Dose CT Actually Show?
A low-dose CT scan is not a full diagnostic scan. It’s designed to find small, early signs of cancer-like tiny nodules in the lungs-without exposing you to much radiation. The dose is about 1.2 millisieverts (mSv), which is roughly one-tenth of a standard chest CT and less than what you’d get from natural background radiation over six months.
During the scan, you lie on a table while the machine takes quick, shallow images of your lungs. No needles, no contrast dye, no fasting. It takes less than 10 seconds. But what happens after matters just as much as the scan itself.
Most scans-about 75%-come back normal. No nodules found. You’re told to come back in a year.
But about 25% of initial scans show something unusual. That doesn’t mean cancer. In fact, 96% of all positive findings turn out to be harmless. These are usually small, non-calcified nodules under 6 mm. They can be caused by old infections, scar tissue, or even dust you breathed in years ago.
Here’s how it works: If a nodule is 4 mm or larger, it’s flagged. If it’s between 4 and 6 mm, you’ll get a follow-up scan in 6 months. If it’s bigger than 6 mm, you’ll likely need a PET scan or biopsy. Only about 1.2% of these small nodules turn out to be cancer over two years.
That’s why the system is built this way: catch the real cancers early, avoid over-treating the harmless ones. But it’s not perfect. A 2023 survey found 42% of people who got a positive result felt anxious for weeks, even months, waiting for answers.
What Happens If Something Is Found?
If your scan shows a nodule, you won’t be handed a diagnosis. You’ll be referred to a team-radiologist, pulmonologist, maybe a thoracic surgeon-who’ll decide the next step based on size, shape, growth rate, and your overall risk.
For nodules under 6 mm: watch and wait. Repeat scan in 6 to 12 months. Most don’t grow. If they do, you move to biopsy or surgery.
For nodules over 8 mm: more aggressive follow-up. PET scan, possibly a biopsy. The goal is to catch cancer before it spreads.
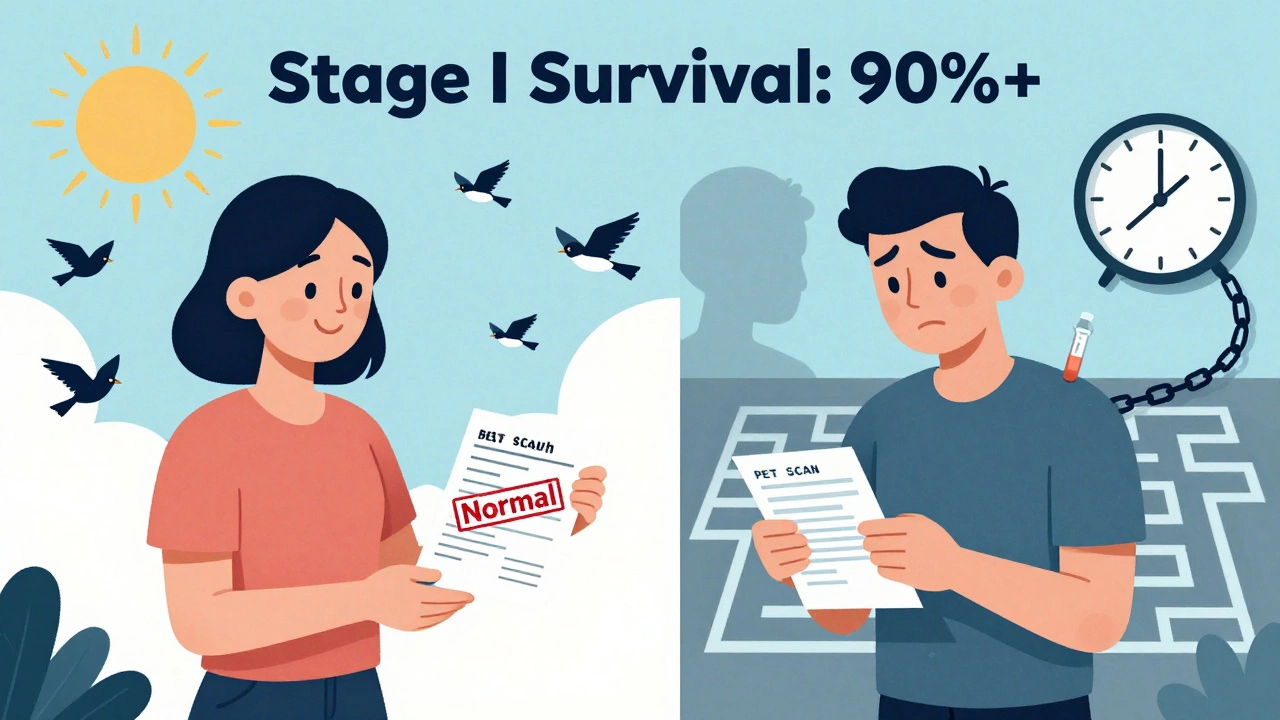
Here’s the good news: if cancer is found early-Stage I-it’s often curable. The NLST study showed that low-dose CT found 3 times more Stage I cancers than chest X-rays. About 71% of cancers caught by screening were at this earliest stage. Surgery, often done with minimally invasive video-assisted techniques, can remove it with a 90%+ survival rate.
One woman from Ohio, Mary Johnson, found her Stage I adenocarcinoma through screening. She had no symptoms. She had no family history. She just smoked for 25 years. “The scan saved me,” she said. “I didn’t even know I had cancer until they told me.”
But not everyone has that outcome. James Wilson, from Texas, had a false positive. Three months, $450 in extra tests, and a lot of sleepless nights before they ruled out cancer. He still gets screened every year-but he doesn’t sleep well the week before.

What Are the Risks?
Yes, there are risks. False positives are the biggest. They lead to anxiety, extra scans, biopsies, and sometimes unnecessary procedures. But the risk of radiation is tiny. The NLST estimated one extra lung cancer death from radiation exposure for every 1,000 people screened. Meanwhile, 15 lung cancer deaths were prevented.
Another risk? Missing the boat. Only about 23% of eligible people in the U.S. get screened. That’s up from 4% in 2016, but it’s still low. Why? Lack of awareness. Fear of results. Cost. And access.
People in rural areas are less likely to get screened. The average distance to a screening center? 32 miles. Many can’t take time off work. Others don’t know their doctor can order the test.
And there’s a racial gap. Black Americans have higher lung cancer rates but are 28% less likely to be screened. That’s not just a statistic-it’s a gap in care.
What About People Who Never Smoked?
Yes, non-smokers get lung cancer. About 10-20% of cases. But low-dose CT screening isn’t recommended for them-yet. The evidence isn’t strong enough to prove it saves lives in this group.
That’s changing. New tools are coming. Blood tests like EarlyCDT-Lung can detect tumor markers before cancer shows up on a scan. AI software can now analyze scans faster and more accurately than humans, reducing false positives by up to 18%. A new risk model called LYFS-CT, tested on over a million veterans, can predict who benefits most from screening-not just by smoking history, but by age, lung function, and other factors.
For now, if you’re a non-smoker with symptoms-coughing up blood, unexplained weight loss, chest pain-see your doctor. You don’t need screening. You need diagnosis.
How Do You Get Started?
It’s not something you can just walk into and ask for. You need a doctor’s order. And before you get the scan, Medicare and most insurers require a counseling session. That’s not a formality. It’s a 25- to 30-minute conversation where your provider explains the benefits, the risks, the chances of false positives, and what happens next.
You should walk out of that visit knowing:
- What your risk is
- What the scan can and can’t find
- What happens if something shows up
- Why quitting smoking still matters-even if you’re being screened
Most clinics now use decision aids-simple tools with pictures and numbers-to help you understand your odds. If your doctor skips this step, ask for it. It’s required for insurance to pay.
And if you’re not sure where to go? Look for an ACR-accredited center. They follow strict standards for radiation dose, image quality, and follow-up protocols. You can find one at acr.org.
What’s Next for Lung Screening?
Medicare is reviewing its rules right now. They’re considering dropping the 15-year quit limit and raising the upper age limit to 80. That could open screening to nearly 20 million people-19% more than current guidelines.
Biennial (every two years) screening is also being studied. The NELSON trial in Europe showed it’s just as effective as annual screening, with fewer false positives. That could make screening more sustainable and less stressful.
But the biggest barrier isn’t science. It’s access. In 41% of U.S. counties, there’s no accredited screening center. That’s not just inconvenient-it’s deadly. If you’re eligible, don’t wait for the system to catch up. Ask your doctor. Push for it. Your lungs might depend on it.
Bottom Line
Low-dose CT screening isn’t for everyone. But if you’re 50 to 80, smoked 20 pack-years or more, and still smoke or quit within the last 15 years-it’s one of the most effective cancer prevention tools we have. It doesn’t prevent cancer. It finds it early, when it’s easiest to cure.
It’s not perfect. False positives happen. Anxiety is real. But the numbers don’t lie: 20% fewer lung cancer deaths. Thousands of lives saved. And for people like Mary Johnson, it meant a second chance.
If you think you qualify, don’t assume someone else will tell you. Talk to your doctor. Get the scan. And if you’ve quit smoking? That’s still a win. But don’t let the 15-year clock be the only thing that decides your fate.





Iris Carmen
11 December, 2025 . 09:05 AM
i got my scan last year and they found a 3mm nodule... turned out to be scar tissue from a bad cold i had in 2010. still freaked me out for 3 months tho 😅
Shubham Mathur
12 December, 2025 . 11:45 AM
Why do they still use 15 years as the cutoff when studies show 1/3 of lung cancers happen after that? The guidelines are outdated and it's killing people who quit smoking but still have risk
Noah Raines
13 December, 2025 . 06:56 AM
my doc tried to skip the counseling session said i 'already knew what i was getting into'... i made him do it anyway. best 30 mins i've spent in a clinic 😎
Sabrina Thurn
15 December, 2025 . 02:16 AM
As a pulmonologist, I can confirm the 96% false positive rate holds up in real-world practice. The key is managing expectations upfront. Most patients panic when they hear 'abnormal finding' without understanding that 'abnormal' ≠ 'cancer'. Structured follow-up protocols reduce anxiety dramatically.
Larry Lieberman
15 December, 2025 . 20:54 PM
I’m 58, smoked 1.5 packs a day for 22 years, quit 18 years ago. My doc says I don’t qualify. I’m getting a second opinion. This feels like ageism + arbitrary cutoffs. 🤔
Brianna Black
16 December, 2025 . 07:42 AM
The disparity in screening access is a national disgrace. I work in public health in rural Kentucky-our nearest accredited center is 72 miles away. Many of our patients have never even heard of low-dose CT. This isn’t just about medicine-it’s about equity.
Chris Marel
17 December, 2025 . 05:31 AM
In Nigeria, we don’t even have CT scanners in most towns. But I read this and thought-maybe we need community education first. If people don’t know screening exists, how can they ask for it? We need to start with awareness, not technology.
Andrea Beilstein
17 December, 2025 . 09:33 AM
There’s something deeply ironic about screening for cancer in a society that won’t fund clean air initiatives or regulate industrial toxins. We’re treating the symptom while ignoring the disease of environmental neglect.
Morgan Tait
18 December, 2025 . 00:09 AM
I’ve been following this for years. Did you know the government quietly funded a secret AI project that can detect cancer from CT scans with 99.1% accuracy? But they won’t release it because it would make radiologists obsolete. And the insurance companies love false positives-they make more money off follow-ups. 🤫
iswarya bala
19 December, 2025 . 14:09 PM
i smoked for 12 years and quit 10 years ago. my mom had lung cancer. i asked for a scan and they said no. i paid out of pocket. found a 4mm nodule. 6 months later it was gone. i’m alive because i didn’t listen to them
Courtney Black
20 December, 2025 . 04:23 AM
The system is designed to make you feel like you’re doing something proactive while actually serving the medical-industrial complex. You get screened. You get anxious. You get more scans. They get paid. You get tired.
Stacy Tolbert
21 December, 2025 . 08:57 AM
I cried after my scan. Not because I was scared of cancer-because I realized I’d spent 20 years hating my body for smoking, and now I was finally doing something to protect it. That scan didn’t just show my lungs. It showed my redemption.
precious amzy
21 December, 2025 . 14:24 PM
One must ask: Is the reduction in mortality statistically significant when weighed against the psychological toll of false positives? The utilitarian calculus of population screening ignores the existential weight borne by the individual. Are we saving lives-or manufacturing suffering?
Nikhil Pattni
22 December, 2025 . 11:40 AM
I read the NLST study and the NELSON trial and the JAMA meta-analysis and the Cochrane review and the 2024 Lancet Oncology paper on AI-assisted nodule detection and let me tell you the current guidelines are based on 2011 data and they’re already obsolete because now we have deep learning models trained on 2 million scans that can predict malignancy with 94% accuracy using only texture analysis and not even size or shape so why are we still using the same 4mm 6mm 8mm thresholds from 13 years ago
Maria Elisha
23 December, 2025 . 00:03 AM
eh i’m 52, smoked 1 pack for 15 years. i’m not getting scanned. too much hassle. if i get cancer i get cancer. no point stressing over it.