When your immune system turns against your own body, it doesn’t just cause discomfort-it can destroy joints, damage organs, and change your life. That’s what happens in autoimmune diseases like rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. For decades, doctors could only treat the pain and swelling. But since the 1980s, a new kind of treatment has emerged: DMARDs. These aren’t just painkillers. They’re designed to stop the damage before it happens.
What Are DMARDs, Really?
DMARD stands for disease-modifying antirheumatic drug. That’s a mouthful, but here’s what it means in plain terms: these drugs change how your immune system behaves. Instead of just masking symptoms like ibuprofen or steroids do, DMARDs slow down or even stop the immune system’s attack on healthy tissue. This can prevent long-term joint damage, reduce flare-ups, and help people stay active for years longer. There are three main types of DMARDs, and they work in very different ways:- Conventional synthetic DMARDs-these are the older, pill-based drugs like methotrexate, leflunomide, and hydroxychloroquine. They work broadly across the immune system.
- Biologic DMARDs-these are newer, targeted therapies made from living cells. They block specific parts of the immune response, like TNF-alpha or IL-6, which are key drivers of inflammation.
- Targeted synthetic DMARDs-these are oral pills like tofacitinib and upadacitinib that block specific enzymes (JAK inhibitors) inside immune cells.
Most rheumatologists start with a conventional DMARD-usually methotrexate-because it’s been used safely for over 40 years. It’s also affordable: generic methotrexate costs as little as $4 a month in the U.S. If that doesn’t control the disease after 3-6 months, they’ll move to a biologic or JAK inhibitor.
How Biologics Are Different
Biologics are not like regular pills. They’re made from proteins that mimic or block parts of your immune system. Think of them as precision missiles instead of a shotgun blast. While conventional DMARDs affect many immune cells, biologics target just one pathway-like TNF-alpha, B-cells, or interleukins. Examples include:- Adalimumab (Humira)-a subcutaneous injection given every other week
- Infliximab (Remicade)-an IV infusion every 8 weeks
- Rituximab (Rituxan)-targets B-cells that produce inflammatory signals
- Tocilizumab (Actemra)-blocks IL-6, a major inflammation trigger
These drugs can bring dramatic relief. One study showed patients with rheumatoid arthritis improved by 70% in joint pain and swelling after six months on a biologic. But they come with trade-offs. Because they’re so specific and powerful, they leave you more vulnerable to infections. That’s why doctors check for tuberculosis and hepatitis before starting treatment-and why you’re told to avoid sick people and wash your hands constantly.
Cost, Access, and Real-Life Challenges
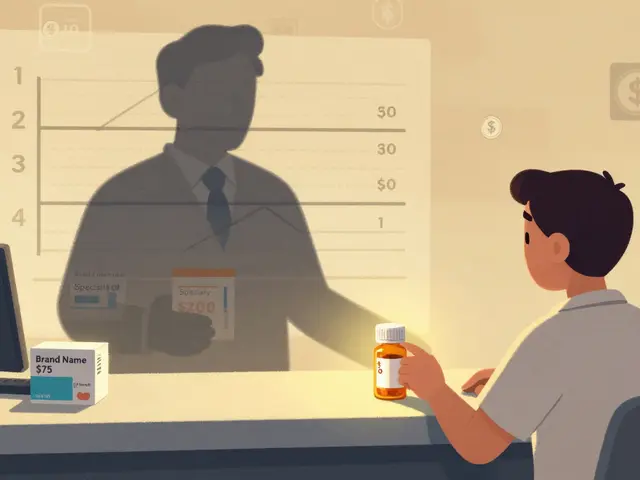
Let’s be honest: biologics are expensive. Without insurance, they can cost $1,000 to $5,000 a month. Even with coverage, many patients pay $500 or more out of pocket. That’s why insurance companies make you try cheaper DMARDs first-and why getting approved can take 2 to 6 weeks. Biosimilars have helped. Since 2016, copycat versions of drugs like adalimumab and etanercept have hit the market. They’re 15-30% cheaper and just as effective. But they’re not available everywhere, and not all insurers cover them equally. Then there’s the daily reality of treatment. Biologics come in pre-filled pens or syringes. You have to learn how to inject yourself-sometimes in your thigh or belly. Many patients feel anxious at first. But with a nurse’s training and a little practice, it becomes routine. Some report mild redness or itching at the injection site, which usually fades.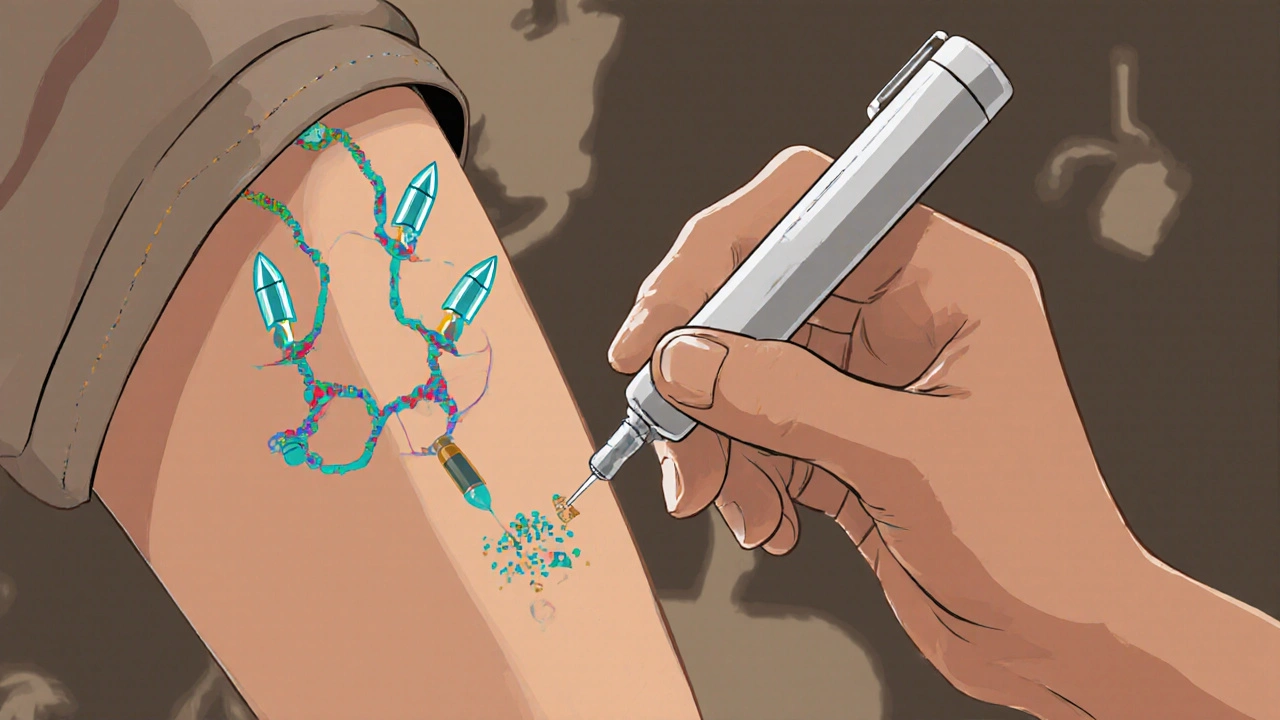
Side Effects and Monitoring
All DMARDs require monitoring. With methotrexate, you’ll get blood tests every 4-8 weeks to check your liver and blood counts. Nausea, fatigue, and mouth sores are common early on, but most people adjust. Taking folic acid daily can reduce these side effects significantly. Biologics don’t need as many blood tests, but infection risk is higher. About 5-10% of users develop serious infections-pneumonia, skin abscesses, even sepsis. That’s why you’re told to call your doctor if you have a fever, sore throat, or unexplained cough. Even a small cut can become a problem if your immune system is suppressed. There’s also a small risk of certain cancers, especially lymphoma, and heart failure in people with existing heart conditions. That’s why the FDA requires black box warnings on all biologics. But for most patients, the benefits outweigh the risks-especially when the alternative is progressive joint destruction.What to Expect Over Time
DMARDs don’t work overnight. Methotrexate can take 6-12 weeks before you feel better. Biologics often act faster-some patients notice improvement in 2-4 weeks. But consistency matters. Missing doses reduces effectiveness. Studies show 30-50% of patients skip doses at least once a month, often because of side effects or cost. If a biologic stops working after a year or two, it’s not unusual. Your body can develop antibodies that neutralize the drug. Doctors may switch you to another biologic or try a JAK inhibitor instead. Upadacitinib, approved in 2019, is one of the newest options-it’s an oral pill that works in 2 weeks and is now approved for both rheumatoid and psoriatic arthritis.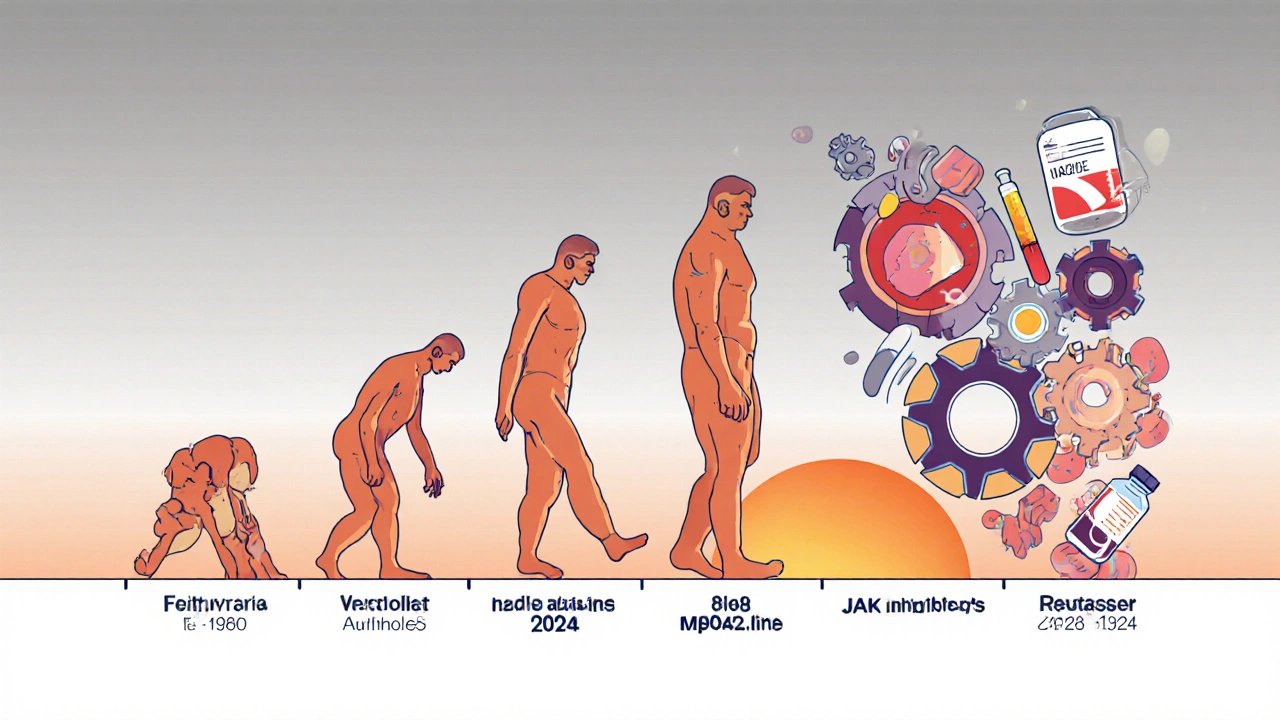
Is This Therapy Right for You?
DMARDs aren’t for everyone. If your disease is mild, you might manage with NSAIDs and physical therapy. But if you have moderate to severe inflammation, joint damage on X-rays, or high levels of inflammatory markers in your blood, DMARDs are the standard of care. The goal isn’t just to feel better today. It’s to protect your body for tomorrow. People who start DMARDs early are far less likely to need joint replacements, lose mobility, or end up disabled. That’s why rheumatologists say: don’t wait. If you’ve had symptoms for more than 6 weeks, get tested.What’s Next?
Research is moving fast. New drugs are in Phase III trials targeting even more specific immune signals, with the aim of reducing infection risk while keeping effectiveness. Some scientists are exploring personalized dosing based on genetics or biomarkers. Others are testing combination therapies that use lower doses of multiple drugs to reduce side effects. For now, DMARDs remain the backbone of autoimmune disease treatment. Whether you’re on a weekly pill or a monthly injection, you’re part of a medical revolution that’s changed the lives of millions. You’re not just managing symptoms-you’re changing the course of your disease.Are DMARDs the same as steroids?
No. Steroids like prednisone reduce inflammation quickly but don’t stop disease progression. They’re used short-term to control flares while DMARDs take effect. Long-term steroid use causes serious side effects like bone loss, weight gain, and diabetes. DMARDs are designed for ongoing use to protect your joints and organs.
Can I stop taking DMARDs once I feel better?
Usually not. Even if your symptoms disappear, the underlying immune dysfunction remains. Stopping treatment often leads to a flare, sometimes worse than before. Some patients in remission may reduce their dose under doctor supervision, but stopping entirely is risky and rarely recommended.
Do biologics weaken my immune system permanently?
No. The effect is temporary and reversible. Once you stop taking a biologic, your immune system gradually returns to its baseline. That’s why infections clear up after treatment ends. But while you’re on it, your body’s ability to fight certain pathogens is reduced, so you need to be cautious.
Why do I need blood tests so often?
DMARDs can affect your liver, kidneys, and bone marrow without causing obvious symptoms. Regular blood tests catch problems early-like low white blood cell counts or elevated liver enzymes-before they become dangerous. Skipping tests increases your risk of serious complications.
Are there natural alternatives to DMARDs?
Diet, fish oil, and turmeric may help reduce inflammation slightly, but none can replace DMARDs in stopping autoimmune damage. There’s no scientific evidence that supplements prevent joint destruction. Relying on them instead of proven treatments can lead to irreversible disability.
What happens if a biologic stops working?
It’s common. Your body may develop antibodies that neutralize the drug. Your doctor will switch you to another biologic with a different target-like moving from a TNF blocker to an IL-6 inhibitor-or try a JAK inhibitor. Most patients respond well to the next option.
Can I get vaccines while on DMARDs?
Yes-but timing matters. Live vaccines (like MMR or shingles) are unsafe while on biologics or high-dose methotrexate. Inactivated vaccines (flu, pneumonia, COVID-19) are safe and strongly recommended. Get them before starting treatment if possible. Always check with your rheumatologist before any vaccine.



dace yates
11 November, 2025 . 01:47 AM
I started methotrexate last year and honestly, I thought I’d hate the injections-but the pen is way easier than I expected. Still, the fatigue is real. Took me three months to feel even a little better. Folic acid? Life saver. I take it like candy now.
David Barry
12 November, 2025 . 06:46 AM
Let’s be real-biologics are just expensive placebos with a side of immunosuppression. You trade one set of problems for another. The ‘miracle drugs’ are just corporate marketing wrapped in clinical jargon. And don’t get me started on the insurance hoops. I’ve seen people wait six months just to get approved. Meanwhile, their joints turn to dust.
Danae Miley
13 November, 2025 . 03:17 AM
David, your cynicism is statistically unfounded. Biologics reduce radiographic progression by 60–80% in RA patients over five years. The risk-benefit ratio is overwhelmingly positive when monitored properly. You’re conflating access barriers with therapeutic failure. That’s not analysis-it’s defeatism.
Elizabeth Buján
15 November, 2025 . 01:03 AM
I get what you're saying, David... but I just wanna say-when I started Humira, I couldn’t tie my shoes. Now I hike every weekend. It wasn’t magic. It was medicine. And yeah, I’m scared of infections, but I’d rather be scared and walking than stuck in a chair. You’re not alone in feeling this way. I cried the first time I injected myself. But I’m still here. And I’m grateful.
Ryan Everhart
15 November, 2025 . 17:34 PM
So if I stop taking my JAK inhibitor, does my immune system just reboot like a Windows PC? Or is it more like a broken toaster that never quite works right again? Asking for a friend who’s considering quitting because the copay is $800.
Samantha Wade
17 November, 2025 . 15:42 PM
Elizabeth, your story is beautiful. And Ryan-yes, your immune system resets. But not instantly. It takes 4–6 weeks for immune cell populations to normalize after stopping a biologic. And no, it doesn’t ‘reboot.’ It relearns. Which is why you need to stay vigilant about infections even after discontinuation. This isn’t a software update-it’s a biological recalibration.
Benjamin Stöffler
17 November, 2025 . 22:02 PM
And yet… we must ask: Is the immune system truly the enemy? Or is it merely misinformed? In the grand tapestry of evolutionary biology, autoimmunity is not a flaw-it is a tragic misalignment of a system designed for survival, now turned inward by modernity’s toxins, sedentary life, and dietary betrayal. Methotrexate? A scalpel in a world that needs a symphony. We treat symptoms, not causes. We silence the alarm, but never fix the broken sensor.
Arpita Shukla
19 November, 2025 . 17:58 PM
Benjamin, you sound like you read a philosophy textbook after a 12-hour rheumatology lecture. The immune system isn’t ‘misinformed’-it’s malfunctioning. And yes, lifestyle matters. But if your joints are already eroding, yoga and kale won’t rebuild cartilage. Methotrexate isn’t a scalpel-it’s a circuit breaker. It stops the fire before the house burns down. You can philosophize after you stop limping.
Charles Lewis
21 November, 2025 . 05:52 AM
Arpita, your experience is a microcosm of the larger truth: early intervention changes trajectories. I’ve worked with patients who waited two years before starting DMARDs-they ended up needing two hip replacements by 45. Those who started within six months of symptom onset? Many are working, traveling, raising kids. The data is clear. The barrier isn’t science-it’s fear, misinformation, and systemic neglect. We need better patient education, not more philosophical debates.
Renee Ruth
22 November, 2025 . 13:27 PM
Ugh. I just got my third biologic rejection this month. Insurance says ‘try another DMARD’-but I’ve been on methotrexate for 18 months and my CRP is still 28. I’m 32. I have two toddlers. I can’t even pick them up without crying. They want me to wait for another ‘trial’? Like I’m some lab rat? I’m not a statistic. I’m a mother. And I’m tired of being told to ‘be patient.’
Mark Rutkowski
22 November, 2025 . 14:28 PM
Renee, I hear you. And I want you to know-you’re not failing. The system is. But your body? It’s still fighting. And you’re still here. That’s courage. I’ve watched patients go from wheelchair to walking with a cane, then to walking without. It’s slow. It’s messy. But it’s possible. You’re not alone in this fight. And if you need someone to scream with you at 2 a.m. about insurance forms? I’m here. You matter more than your lab values.
Alyssa Lopez
24 November, 2025 . 13:12 PM
Just sayin’ if you’re on biologics in the US you’re basically a walking biohazard. Why don’t we just quarantine the whole autoimmune community? No seriously, my cousin got pneumonia from a flu shot while on Humira. The docs said ‘it’s normal.’ Normal? That’s not normal. That’s negligence. We need to stop this biologic madness before it turns into a pandemic of immunosuppressed zombies.