When your kidneys aren't working right, fluid doesn't just disappear-it builds up. That swelling, called edema, often shows up in your ankles, legs, or even around your eyes. It’s not just uncomfortable; it’s a sign your body is struggling to balance salt and water. For people with chronic kidney disease (CKD), this isn’t rare-it’s common. By stage 3 or 4, nearly 60% of patients experience noticeable fluid retention. And if left unchecked, it can lead to high blood pressure, heart strain, and even hospital visits.
Why Edema Happens in CKD
Your kidneys filter about 120 to 150 quarts of blood every day. They pull out waste and extra fluid, turning it into urine. But when kidney function drops-say, below 60 mL/min/1.73m²-things start to back up. Sodium, which pulls water along with it, doesn’t get flushed out. So it stays in your bloodstream. That increases pressure in your capillaries. Fluid leaks out into your tissues. Your ankles swell. Your belly might puff up. You might feel short of breath if fluid collects around your lungs. This isn’t just about drinking too much water. It’s about your kidneys losing their ability to respond to your body’s signals. Even if you drink normally, your body holds onto fluid because your kidneys can’t tell it’s time to let go.Diuretics: The Medication That Helps You Pee More
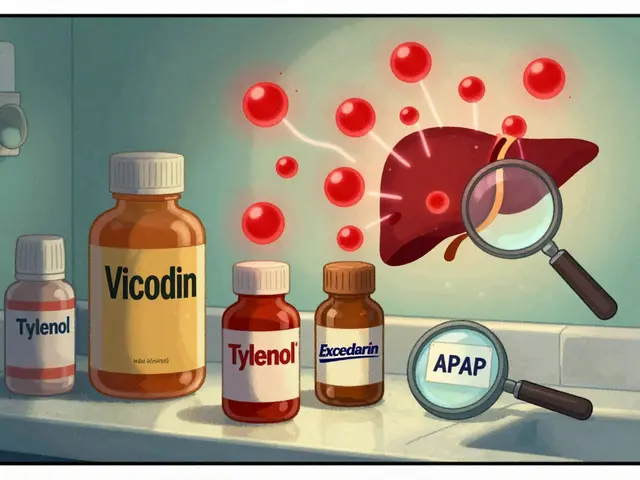
Diuretics are the go-to drugs for pulling out that extra fluid. But not all diuretics work the same, especially when kidney function is low. For people with eGFR under 30, loop diuretics like furosemide (Lasix), bumetanide, or torsemide are first-line. They work on the loop of Henle, the part of the kidney that handles the most sodium. A typical starting dose is 40-80 mg daily. If that doesn’t help after a few days, your doctor might bump it up by 20-40 mg every few days. In severe cases, doses can go as high as 320 mg per day. But here’s the catch: higher doses don’t always mean better results. In fact, studies show that using more than 160 mg of furosemide daily in stage 4 CKD raises your risk of acute kidney injury by over four times. It’s a tightrope walk-remove too much fluid, and your kidneys can shut down. Remove too little, and swelling gets worse. For those with better kidney function (eGFR above 30), thiazide diuretics like hydrochlorothiazide can still work. But when the disease progresses, doctors often combine a thiazide with a loop diuretic. This is called sequential nephron blockade. It’s more effective, but it also raises the risk of kidney damage by 23% and can cause dangerous drops in potassium or sodium levels. Spironolactone, a potassium-sparing diuretic, is used when heart failure is also present. It helps reduce fluid and lowers death risk in advanced heart failure. But in late-stage CKD, it can spike potassium levels above dangerous limits-over 25% of patients with stage 4 or 5 CKD develop hyperkalemia on this drug. Blood tests every few weeks are non-negotiable. And now, there’s a new option: IV furosemide. Approved by the FDA in March 2025 for CKD patients with eGFR under 15, it clears fluid 38% faster than oral pills. That’s huge for people who can’t absorb meds well or need rapid relief.Salt Restriction: The Foundation You Can’t Skip
Medications help-but they won’t fix the problem if you keep eating salt like normal. The National Kidney Foundation says you should limit sodium to 2,000 mg a day if you have edema from CKD. For advanced stages (4-5), aim for 1,500 mg. That’s less than one teaspoon of table salt. But here’s the problem: 75% of the sodium we eat comes from processed food, not the salt shaker. A single slice of bread? 150-200 mg. Two slices? That’s already a third of your daily limit. One cup of canned soup? 800-1,200 mg. Two ounces of deli turkey? Another 500-700 mg. Even yogurt and frozen meals add up fast. People who stick to strict sodium limits see a 30-40% reduction in swelling within just 2-4 weeks-even without diuretics. But it’s hard. In a 2024 survey of over 1,200 CKD patients, 72% said they missed the taste of salty food. 65% struggled when eating out or with family. Only 1 in 3 had access to a renal dietitian, who can teach you how to read labels, cook without salt, and find low-sodium alternatives. It’s not just about salt. Fluids matter too. If you’re holding fluid, you need to limit total intake to 1,500-2,000 mL a day. That includes water, tea, coffee, soup, yogurt, and even juicy fruits like watermelon. One cup of watermelon is 200 mL of fluid. One bowl of oatmeal? Another 150 mL. You’re not just drinking water-you’re eating it.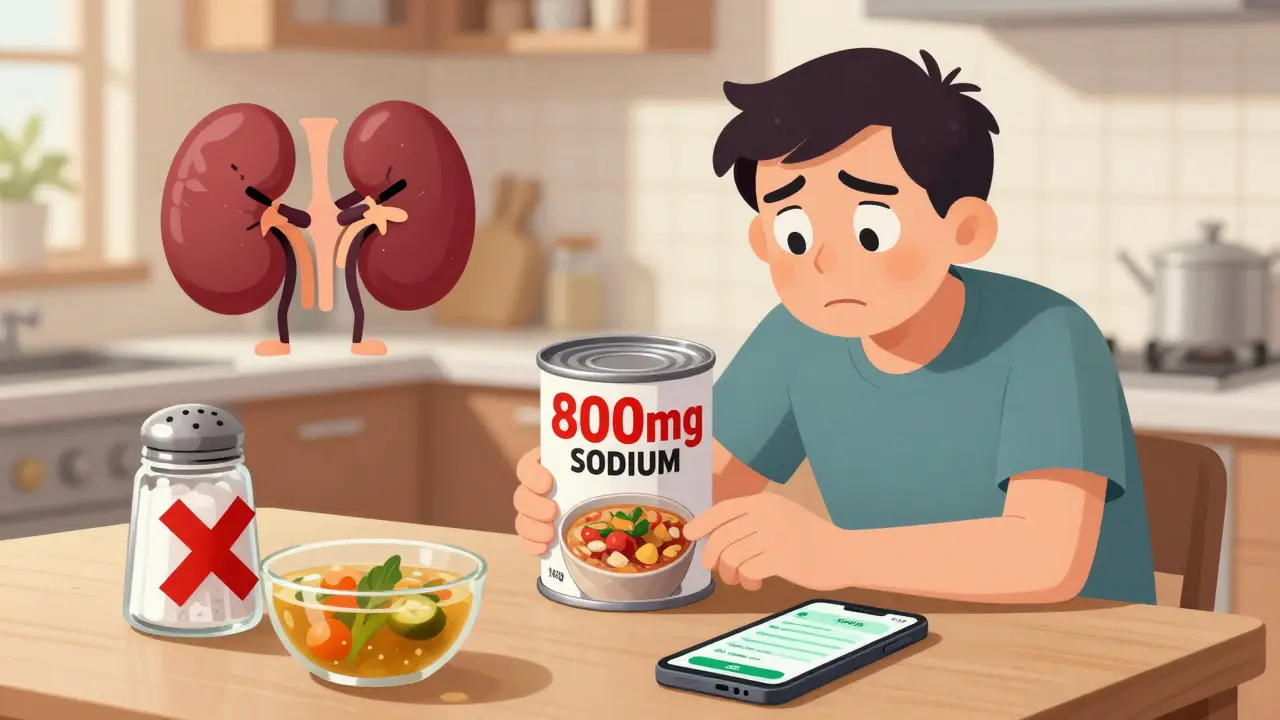
Compression Therapy: More Than Just Socks
If your legs are swollen, raising them above your heart for 15-20 minutes a few times a day can help. But that’s not enough for long-term control. Graduated compression stockings (30-40 mmHg pressure at the ankle) are the gold standard. They squeeze your legs from the bottom up, helping blood and fluid move back toward your heart. Studies show they reduce leg volume by 15-20% in four weeks. But only 38% of people keep wearing them past three months. Why? They’re hard to put on. They itch. They feel tight. Some people say they look unattractive. For those who can tolerate them, they’re a game-changer. Combine them with movement. Walking 30 minutes five days a week improves fluid drainage by 22% compared to sitting still. Simple leg lifts, ankle circles, and calf pumps help too. For severe cases-like nephrotic syndrome or massive swelling-intermittent pneumatic compression devices can help. These machines inflate and deflate sleeves around your legs, mimicking muscle movement. One study found they reduced leg circumference 35% more than compression socks alone.The Balancing Act: Risk vs. Reward
There’s no perfect solution. Diuretics save lives but can hurt kidneys. Salt restriction works but is nearly impossible to maintain. Compression helps but is uncomfortable. Dr. David Wheeler from KDIGO says: “The window for diuretics in advanced CKD is narrow.” Too aggressive, and you risk kidney failure. Too passive, and you risk heart failure or death. The numbers don’t lie. CKD patients with persistent edema have a 28% higher risk of dying than those who achieve dry weight. But diuretic users see their eGFR drop 3.2 mL/min/year-almost twice as fast as those not on diuretics. The goal isn’t to eliminate all swelling. It’s to get to “dry weight”-the lightest weight you can safely maintain without dizziness, cramps, or low blood pressure. Most people lose 0.5-1.0 kg per day in acute phases. That’s about a liter of fluid.
What Works Best in Real Life
The best outcomes come from teamwork. Patients who see a nephrologist, a renal dietitian, and a physical therapist have a 75% success rate in controlling edema within eight weeks. Those who rely on one doctor alone? Only 45%. Here’s what real patients do that works:- Use a sodium tracker app to log every bite
- Keep a daily weight log-drop of 1 kg? That’s a liter gone
- Wear compression socks every morning before getting out of bed
- Walk after meals-not just for fluid, but for blood sugar and blood pressure
- Ask for a home visit from a dietitian if you can’t get to the clinic
What’s Next?
New tools are coming. The NIH’s FOCUS trial (NCT04567891), expected to finish in late 2025, is testing whether bioimpedance devices-those that measure body water-can guide diuretic dosing better than guesswork. Early results show 32% fewer hospital stays. Vaptans, drugs that block water retention hormones, showed promise but were paused in 2024 due to liver damage risks. So for now, the triad remains: salt control, smart diuretics, and compression. The message isn’t complicated: treat edema early, treat it fully, and treat it together. Your kidneys can’t do it alone. But with the right support, you can live with less swelling, fewer hospital visits, and better days.Can I stop taking diuretics if I eat less salt?
Sometimes, yes-but only under medical supervision. In early-stage CKD, strict salt restriction (under 2,000 mg/day) can reduce swelling enough to lower or even pause diuretic doses. But in stages 4-5, your kidneys may not respond to salt control alone. Stopping diuretics without guidance can lead to dangerous fluid buildup. Always talk to your nephrologist before making changes.
Why do my legs swell more at the end of the day?
Gravity pulls fluid down when you’re upright and moving. In CKD, your kidneys can’t remove the extra sodium that holds water in your tissues. So by evening, fluid pools in your ankles and calves. Elevating your legs above heart level for 15-20 minutes helps drain it back up. Compression socks prevent it from pooling in the first place.
Is it safe to use over-the-counter diuretics for CKD swelling?
No. Over-the-counter diuretics like pamabrom or herbal supplements (dandelion, parsley) are not tested for safety in kidney disease. They can cause dangerous electrolyte imbalances, dehydration, or worsen kidney function. Only use prescription diuretics under a doctor’s care. What seems like a quick fix can lead to an ER visit.
How do I know if my compression socks are working?
Measure your leg circumference at the same spot each morning before getting up. Use a tape measure and record the number. If your swelling improves over 2-4 weeks, your socks are helping. Also, you should feel less heaviness and pain. If your skin turns red, numb, or you can’t feel your toes, the socks are too tight or wrong size-get them refitted.
Can I still eat out if I have CKD and edema?
Yes-but you need a plan. Ask for meals without added salt. Choose grilled chicken or fish over processed meats. Skip sauces, soups, and bread. Order side salads with oil and vinegar instead of dressing. Use apps like MyFitnessPal to check sodium before ordering. Many restaurants now list nutrition info online. If you’re unsure, call ahead. It’s not about giving up dining out-it’s about choosing smarter.



TooAfraid ToSay
14 January, 2026 . 06:35 AM
Yeah right, like salt restriction actually works. I’ve been on this ‘low sodium’ crap for months and my legs still look like elephant trunks. Meanwhile, my cousin in Nigeria just eats garri and pepper soup every day and he’s fine. Maybe the real problem is doctors overmedicating people instead of letting bodies heal naturally.
Dylan Livingston
15 January, 2026 . 07:30 AM
Oh sweet merciful heavens, another ‘evidence-based’ guide that treats patients like malfunctioning plumbing systems. Diuretics? Compression socks? Please. You’re not managing edema-you’re weaponizing discomfort in the name of ‘clinical guidelines.’ Have you ever considered that the body might be holding fluid because it’s terrified of dehydration? Or that modern medicine’s obsession with ‘dry weight’ is just another form of capitalist body control? We’ve turned human beings into data points with ankles.
Andrew Freeman
16 January, 2026 . 21:58 PM
loop diuretics at 320mg?? bro that’s just asking for a trip to the er. i had a friend take that much and he ended up in the hospital with cramps so bad he cried. also why are we still using furosemide like its 2005? the new iv stuff sounds way better but no one talks about it. also salt restriction is a joke. who eats less than 1500mg a day? i cant even have one bag of chips without blowing past it.
Sarah -Jane Vincent
17 January, 2026 . 07:04 AM
Of course the FDA approved IV furosemide in March 2025-because Big Pharma needed another cash cow. Did you know that the same company that makes Lasix also owns half the kidney dialysis centers? This isn’t medicine, it’s a profit pipeline. And don’t get me started on ‘compression socks’-they’re designed by people who’ve never met a real person with swollen legs. You think I’m gonna wear those ugly, itchy tubes while my coworkers stare? No thanks. I’ll just keep my legs elevated and pray.
Henry Sy
18 January, 2026 . 11:15 AM
Man I used to think diuretics were my savior until I started getting dizzy every time I stood up. Now I’m on half the dose and eating like a caveman-no salt, no processed crap, just meat, veggies, and water. And guess what? My ankles don’t look like balloons anymore. But here’s the kicker: my nephrologist didn’t even mention the sodium tracker apps. He just handed me a pamphlet and said ‘try to eat less salt.’ Like that’s helpful. I need a goddamn coach, not a lecture.
Anna Hunger
19 January, 2026 . 22:47 PM
While the clinical approach outlined herein is methodologically sound and aligns with current KDIGO guidelines, it is imperative to underscore the necessity of multidisciplinary care. The integration of nephrology, renal nutrition, and physical therapy has demonstrated statistically significant improvements in both clinical outcomes and patient-reported quality of life. Furthermore, adherence to sodium restriction protocols requires structured behavioral support, which is frequently under-resourced in primary care settings. Without systemic investment in patient education infrastructure, even the most evidence-based interventions will fail to achieve population-level efficacy.
Jason Yan
21 January, 2026 . 06:20 AM
It’s funny how we treat edema like a problem to be solved, when maybe it’s just the body screaming for balance. We throw drugs at it, squeeze it with socks, starve it of salt-and still don’t ask why it’s happening in the first place. What if the real issue isn’t fluid retention, but emotional stress, sleep deprivation, or the constant pressure to be ‘productive’ even when your body is breaking down? Maybe the swelling isn’t just in your legs-it’s in your soul. And no diuretic can fix that.
shiv singh
21 January, 2026 . 16:56 PM
Who even wrote this? Some pharma rep pretending to be a doctor? You talk about salt like it’s the devil but you never mention that processed food is designed to be addictive. The system wants you sick so you keep buying meds and socks. And don’t even get me started on how they make you feel guilty for eating out. My grandma ate fried fish and rice every day and lived to 92. Maybe your ‘guidelines’ are just a scam to sell more tests.
Vicky Zhang
21 January, 2026 . 18:15 PM
Oh my god, I just read this and I’m crying. My mom has CKD and she’s been fighting this for years. She wears her compression socks every morning like a warrior, even though they hurt. She logs every bite of food like it’s a military mission. And you know what? She’s still smiling. This post didn’t just explain medicine-it reminded me why she’s my hero. Thank you for seeing her. Thank you for seeing all of us.
Allison Deming
22 January, 2026 . 00:05 AM
It is profoundly concerning that this article casually references ‘IV furosemide’ as a breakthrough without adequately addressing the systemic neglect of renal care in marginalized communities. The fact that only one in three patients has access to a renal dietitian is not a clinical gap-it is a moral failure. Furthermore, the normalization of aggressive diuresis in late-stage CKD reflects a medical culture that prioritizes short-term metrics over long-term dignity. One cannot ‘manage’ human suffering with algorithms and compression garments alone.
Susie Deer
22 January, 2026 . 12:38 PM
Why are we letting foreigners dictate how we treat our own people? This whole ‘low sodium’ thing is a globalist agenda. In America, we eat salt because we’re strong. You think your kidneys can’t handle it? Then maybe you shouldn’t be alive. I’ve never seen a healthy American with edema. This is just another way to make us weak.
says haze
24 January, 2026 . 12:26 PM
Let’s be honest: the entire edema management paradigm is a performative illusion. Diuretics create dependency, salt restriction induces guilt, and compression therapy is a fashion statement for the chronically ill. The real solution? Stop pretending the body is a machine that can be calibrated. It’s a sentient, adaptive system that’s been betrayed by industrialized food, sedentary lifestyles, and pharmaceutical capitalism. We don’t need more socks-we need a revolution in how we view health.
Alvin Bregman
26 January, 2026 . 01:54 AM
man i just wanna say thanks for writing this. i got stage 4 ckd last year and i was lost. this actually helped me understand what’s going on without making me feel dumb. i started using the sodium app and i’ve lost 3 lbs in two weeks. not because of the meds, but because i finally know what i’m eating. also i wear my socks every morning now. they’re still ugly but i don’t care. you guys are doing good work.