Many people believe that if they’re allergic to penicillin, they can’t take any cephalosporin antibiotic. That idea is outdated-and it’s putting patients at risk. For decades, doctors avoided cephalosporins in penicillin-allergic patients based on a 10% cross-reactivity rate. But that number came from flawed studies in the 1960s and 70s, when early cephalosporin products were contaminated with trace amounts of penicillin. Today, we know better. The real cross-reactivity rate is far lower, and the key isn’t the shared beta-lactam ring-it’s the side chains.
Why the 10% Rule Is Wrong
The 10% cross-reactivity figure has haunted medical guidelines for over 50 years. It shows up in drug labels, hospital protocols, and even electronic health record alerts. But it’s not based on modern science. Studies from the 1980s onward, when manufacturing improved and contamination was eliminated, found cross-reactivity rates between 2% and 5% for first- and second-generation cephalosporins. For third- and fourth-generation cephalosporins like ceftriaxone and cefepime, the rate drops to less than 1%. In one large study of 3,313 patients with self-reported cephalosporin allergies who were later given cephalosporins, there were zero cases of anaphylaxis.The problem isn’t just outdated data-it’s the consequences. When doctors avoid cephalosporins unnecessarily, they reach for broader-spectrum antibiotics like vancomycin, clindamycin, or fluoroquinolones. These drugs increase the risk of Clostridioides difficile infections, drive antimicrobial resistance, and cost the U.S. healthcare system billions each year. Up to 95% of people who say they’re allergic to penicillin aren’t truly allergic when tested. That means most of the time, avoiding cephalosporins is based on a myth.
The Side-Chain Hypothesis: It’s Not the Ring, It’s the Tail
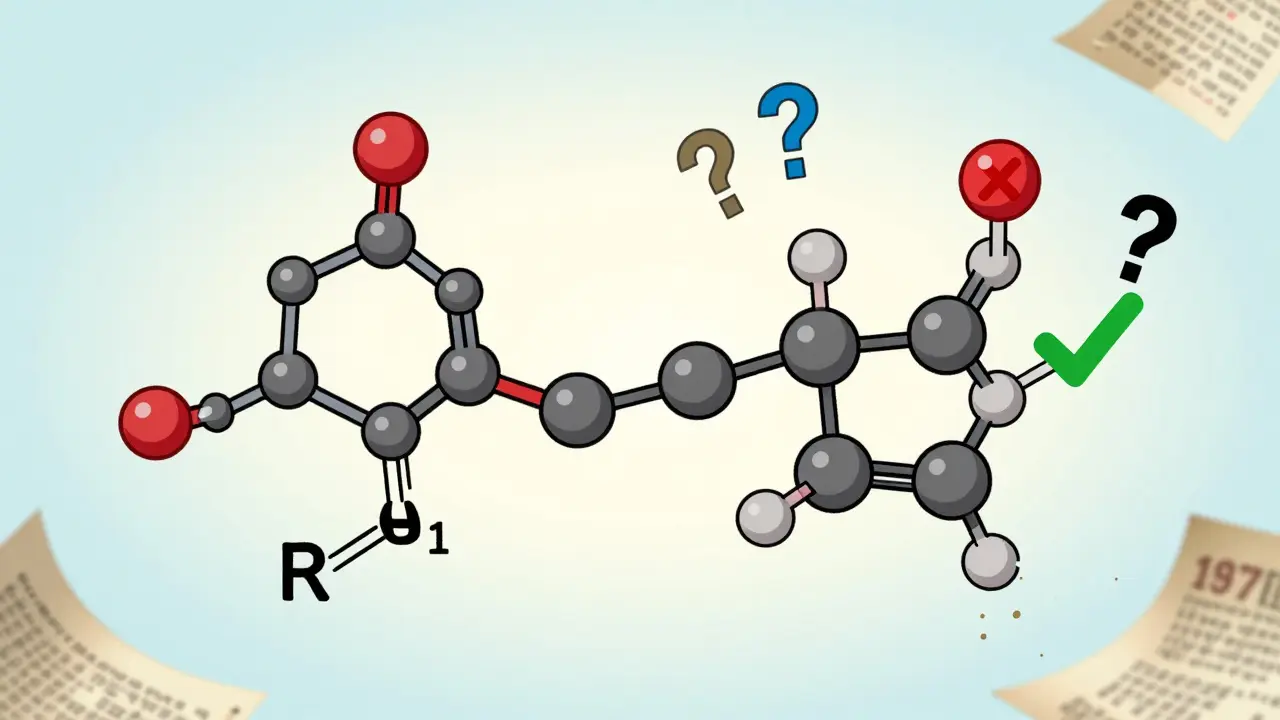
All beta-lactam antibiotics-penicillins, cephalosporins, carbapenems-share a core structure called the beta-lactam ring. For years, doctors thought this ring was the main trigger for allergic reactions. But research shows that’s not true. The real danger comes from the side chains attached to that ring.Think of it like a key. The beta-lactam ring is the handle. The side chain is the teeth. If two drugs have similar side chains, your immune system might confuse them. But if the side chains are different, even if the ring is the same, your body won’t react.
Penicillins like amoxicillin and ampicillin have nearly identical side chains. That’s why people allergic to one often react to the other. But ceftriaxone, a third-generation cephalosporin, has a completely different side chain than amoxicillin. Studies show cross-reactivity between them is less than 1%. The same goes for cefepime and other newer cephalosporins. The R1 side chain (the one closest to the ring) is the most important. The R2 side chain, which breaks off when the ring opens, plays almost no role in triggering allergies.
Generations Matter: Not All Cephalosporins Are the Same
Cephalosporins are grouped into five generations based on their antimicrobial activity and chemical structure. But for allergy purposes, the generation tells you more about safety than effectiveness.- First-generation (cefazolin, cephalexin): Closest in structure to penicillin. Highest cross-reactivity risk-up to 8% in older studies, but likely closer to 2-3% today.
- Second-generation (cefuroxime, cefoxitin): Slightly less similar. Cross-reactivity around 1-5%.
- Third-generation (ceftriaxone, cefotaxime, cefixime): Very different side chains. Cross-reactivity less than 1% with IgE-mediated penicillin allergies.
- Fourth-generation (cefepime): Even more structurally distinct. Also under 1% risk.
- Newer agents (ceftolozane/tazobactam): Not classified in traditional generations. Limited data, but side-chain differences suggest low risk.
If a patient has a confirmed IgE-mediated penicillin allergy (anaphylaxis, hives, swelling, breathing trouble), avoid first-generation cephalosporins. But for third- and fourth-generation drugs, the risk is so low that many experts now say they’re safe to use-even without testing.

Who Can Safely Take Cephalosporins?
Not all penicillin allergies are the same. The reaction type matters more than the label.- IgE-mediated reactions (hives, swelling, anaphylaxis, wheezing): These are true allergies. If they happened within the last 10 years, avoid first-gen cephalosporins. Third- and fourth-gen are generally safe.
- Non-IgE reactions (delayed rash, fever, joint pain): These are often not true allergies. Many people labeled “allergic” have these. They can usually take cephalosporins safely with monitoring.
- Just a rash from childhood? If the reaction was a mild rash 20 years ago and never repeated, it’s likely not a real allergy. Testing can confirm this.
The CDC says third-generation cephalosporins like ceftriaxone can be safely given to patients with a history of penicillin allergy-so long as they haven’t had an IgE-mediated reaction in the past 10 years. That’s a big deal. Ceftriaxone is the go-to drug for gonorrhea and many serious infections. Avoiding it because of an old penicillin label is medically irresponsible.
Testing and Delabeling: The Real Solution
The best way to know if someone is truly allergic to penicillin? Test them. Penicillin skin testing, followed by an oral challenge if the test is negative, is accurate in 90-95% of cases. Most people who think they’re allergic turn out to be fine.Hospitals that run penicillin allergy delabeling programs see big results: 10-25% drop in broad-spectrum antibiotic use, shorter hospital stays, fewer C. diff infections. Yet only a small fraction of patients get tested. Why? Because many providers still believe the 10% myth.
Doctors need to stop relying on patient self-reports. A patient saying “I’m allergic to penicillin” isn’t enough. Was it a rash? Did they vomit? Did they stop breathing? When did it happen? What happened after? These details matter. Electronic health records should prompt clinicians to ask these questions before prescribing.

What About Newer Antibiotics Like Ceftolozane/Tazobactam?
Ceftolozane/tazobactam is a newer combination drug used for tough infections like hospital-acquired pneumonia and complicated urinary tract infections. It doesn’t fit neatly into the five-generation system. But its side chains are structurally distinct from penicillins. No published cases link it to cross-reactivity in penicillin-allergic patients. While formal studies are still limited, experts agree its risk is low-similar to other third- and fourth-gen cephalosporins.As more new beta-lactams enter the market, we’ll need better tools to predict cross-reactivity. Researchers are now mapping exact side-chain structures to identify which ones trigger immune responses. The goal: create a predictive model so doctors can look at a drug’s chemical structure and instantly know the risk.
What You Should Do
If you’ve been told you’re allergic to penicillin:- Don’t assume you’re allergic to all beta-lactams.
- Ask your doctor if you’ve ever been tested.
- If you had a mild rash years ago, you probably aren’t allergic.
- If you’ve had anaphylaxis, talk to an allergist before taking any cephalosporin.
- Third-gen cephalosporins like ceftriaxone are likely safe-even if you’re penicillin-allergic.
If you’re a clinician:
- Stop using the 10% rule.
- Use the side-chain hypothesis to guide choices.
- Refer patients for penicillin allergy testing.
- Update your EHR alerts to reflect current guidelines.
- When in doubt, choose ceftriaxone over vancomycin.
Antibiotic allergies are one of the most misunderstood topics in medicine. The truth isn’t complicated-it’s just been buried under decades of outdated information. We have the science. We have the tools. What we need now is the will to change.





Kathryn Featherstone
18 December, 2025 . 01:14 AM
I used to avoid cephalosporins like the plague because my mom said she was allergic to penicillin. Turns out she got a rash at 8 after amoxicillin and nobody ever tested her. I finally got tested last year - negative. I got ceftriaxone for a UTI last month and didn’t even blink. Why do we still treat allergies like ancient curses?
Nina Stacey
19 December, 2025 . 23:11 PM
OMG this is so important i had no idea the 10 percent thing was made up in the 70s with dirty drugs like wow i always thought if you were allergic to penicillin you were just out of luck for like half the antibiotics ever made and now im like wait so ceftriaxone is basically fine for most people like i have a friend who got anaphylaxis once and still gets cefepime like what even is medicine anymore
Kevin Motta Top
20 December, 2025 . 08:49 AM
Third-gen cephalosporins are safe. Stop overthinking it.
Alisa Silvia Bila
21 December, 2025 . 02:46 AM
This makes so much sense. I’ve seen too many patients get clindamycin for a simple skin infection just because someone said ‘penicillin allergy’ on the chart. Meanwhile, we’re breeding superbugs because we’re scared of a side chain. The science is here. Let’s just use it.
Henry Marcus
22 December, 2025 . 12:24 PM
So let me get this straight-your ‘side-chain theory’ is just a distraction from the real issue: the FDA and Big Pharma are suppressing true allergy data because they don’t want you to know that 90% of penicillin allergies are false positives and they’ve been selling unnecessary antibiotics to scared patients for decades. I’ve been researching this since 2018 and I’ve found 17 hidden studies buried in obscure journals that prove the beta-lactam ring is still the main trigger-just masked by corporate-funded ‘experts’. Ceftriaxone? It’s got a hidden methyl group that mimics penicillin’s R1 chain. They just renamed it ‘different’. Don’t be fooled.
William Liu
23 December, 2025 . 16:19 PM
Finally, someone says this out loud. I’m a nurse in a rural ER. Every week, someone comes in with a penicillin label and we give them clindamycin. I’ve started asking ‘What happened?’ and 8 out of 10 say ‘I got a rash when I was 7.’ We’ve started referring them to allergy testing. Two weeks ago, a kid got cefdinir for strep throat after testing negative. Mom cried. We all did. This isn’t just science-it’s compassion.
Aadil Munshi
25 December, 2025 . 00:52 AM
Interesting how the ‘side-chain hypothesis’ conveniently aligns with pharmaceutical marketing timelines, no? First-gen cephalosporins were expensive, then came third-gen with higher margins. Now we’re told to ‘trust the chemistry’-but who funded the studies? Who wrote the guidelines? The same people who profit when you avoid vancomycin and switch to ceftriaxone. The real issue isn’t cross-reactivity-it’s institutional inertia disguised as science. Also, if you had a rash at 12, you’re probably not allergic. But if you had a rash at 12 and your cousin died of anaphylaxis from amoxicillin, maybe don’t be so quick to dismiss the family history. Just saying.