Uveitic Glaucoma – What You Need to Know
If you have uveitis, you’ve probably heard doctors mention glaucoma as a possible complication. That combo is called uveitic glaucoma. It’s a type of secondary glaucoma that shows up when inflammation inside the eye blocks fluid flow, raising the pressure. The higher pressure can damage the optic nerve and steal your sight if you don’t act fast.
Why Uveitic Glaucoma Happens
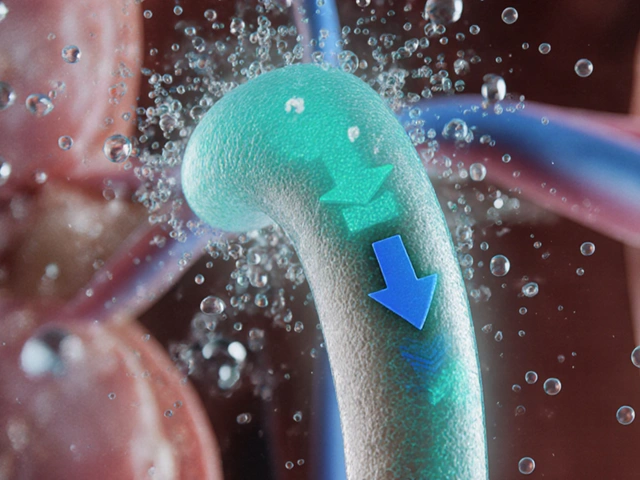
Uveitis is inflammation of the uvea, the colorful middle layer of the eye. When inflamed, cells and proteins flood the front part of the eye and can clog the trabecular meshwork – the tiny drainage system that normally lets fluid drain out.
That clogging makes the fluid (aqueous humor) build up, pushing the pressure up. In some cases, steroid eye drops used to treat uveitis can also raise pressure, adding another risk factor. The danger is that the optic nerve, which sends visual signals to your brain, gets squeezed and starts to deteriorate.
Typical signs include blurry vision, eye pain, halos around lights, and a red eye that doesn’t improve with usual uveitis treatment. Some people notice a sudden drop in peripheral vision – that’s a red flag that the glaucoma is already hurting the optic nerve.
Managing the Condition
First thing doctors do is confirm the diagnosis. A quick eye pressure check (tonometry) tells you if the pressure is high. They’ll also look at the angle of the eye with a gonioscope to see how blocked it is. Imaging tests like OCT (optical coherence tomography) can show early nerve damage.
Treatment has two goals: calm the inflammation and lower the pressure. For the inflammation, doctors might prescribe steroid eye drops, but they’ll keep a close eye on the pressure because steroids can make it worse. Non‑steroidal drops or oral medications are sometimes used to spare the eye from steroid side effects.
Pressure‑lowering meds come in several classes. Beta‑blockers, prostaglandin analogs, carbonic anhydrase inhibitors, and alpha‑agonists each work differently, so doctors often combine them for the best effect. If drops aren’t enough, laser procedures like selective laser trabeculoplasty (SLT) can open the drainage pathways.
When medication and laser fail, surgery becomes the last resort. Options include trabeculectomy (creating a new drainage channel) or tube shunt implants. These surgeries carry risks, but they’re often the only way to stop pressure from soaring.
Living with uveitic glaucoma means regular eye checks. Even if your pressure looks normal now, inflammation can flare up later and push the pressure back up. Keep a symptom diary – note any new pain, vision changes, or red eyes, and call your eye doctor right away.
Side‑step triggers when you can. Some infections, eye injuries, or autoimmune flares provoke uveitis. Managing underlying conditions like rheumatoid arthritis or sarcoidosis can reduce flare‑ups and, in turn, lower glaucoma risk.
Don’t forget lifestyle tweaks. Staying hydrated helps eye fluid balance, and a low‑salt diet can modestly support eye pressure. Avoid smoking – it worsens inflammation and blood flow to the optic nerve.
In short, uveitic glaucoma is avoidable damage if you catch it early and stick to treatment. Talk to your eye doctor about a personalized plan, keep up with appointments, and watch for any changes in your vision. Acting now gives you the best chance to keep your sight clear for years to come.
High Eye Pressure and Uveitis: Causes, Risks, and Treatment Options
Understand how uveitis raises eye pressure, warning signs of a spike, treatments that help (and those to avoid), and smart steps to protect vision.
View More