When you’re taking etodolac for pain or inflammation, you might not think about what else is in your medicine cabinet. But mixing it with other drugs can turn a simple pain reliever into a risk factor. Etodolac is an NSAID - a nonsteroidal anti-inflammatory drug - and like all NSAIDs, it doesn’t play well with everything. Some combinations can raise your blood pressure, hurt your kidneys, or even cause dangerous bleeding. You don’t need to avoid all other meds, but you do need to know which ones to watch out for.
Etodolac and Blood Pressure Medications
If you’re on medication for high blood pressure - like ACE inhibitors (lisinopril), ARBs (losartan), or beta-blockers (metoprolol) - etodolac can make them less effective. This isn’t just a minor issue. A 2023 study in the Journal of Clinical Hypertension found that NSAIDs like etodolac reduced the blood pressure-lowering effect of ACE inhibitors by up to 30% in older adults. That means your blood pressure could creep up without you realizing it, increasing your risk of stroke or heart attack.
Diuretics (water pills) like furosemide or hydrochlorothiazide are another concern. Etodolac reduces blood flow to the kidneys, which makes it harder for diuretics to do their job. The result? Fluid retention, swelling in your legs, and higher blood pressure. If you’re on these meds and start taking etodolac, monitor your weight daily. A sudden gain of 2 kg or more in a week is a red flag.
Etodolac and Other NSAIDs or Aspirin
Don’t take etodolac with ibuprofen, naproxen, diclofenac, or even low-dose aspirin unless your doctor says it’s safe. Combining NSAIDs doesn’t give you better pain relief - it just doubles the risk of stomach ulcers and internal bleeding. A 2024 analysis from the Australian Therapeutic Goods Administration showed that people who took two NSAIDs together had a 4.5 times higher risk of gastrointestinal bleeding than those who took just one.
Even if you’re only taking aspirin for heart protection, it’s still risky. Etodolac can block aspirin’s ability to protect your heart by interfering with how it binds to platelets. If you’re on daily low-dose aspirin for heart disease, talk to your doctor before starting etodolac. You might need to space them out by several hours, or switch to a different pain reliever like acetaminophen.
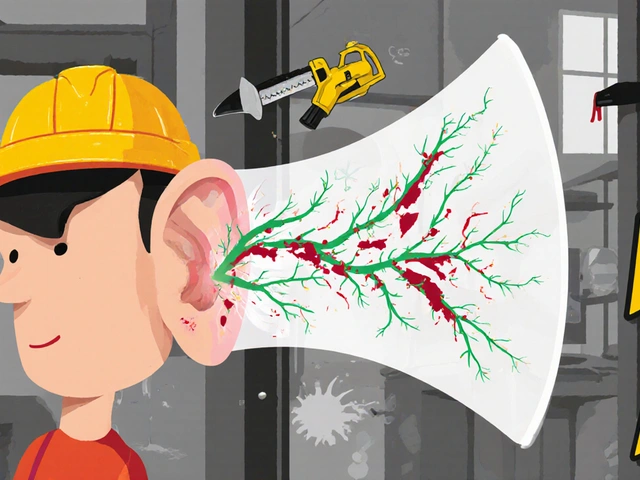
Etodolac and Anticoagulants (Blood Thinners)
If you’re taking warfarin, apixaban, rivaroxaban, or dabigatran, etodolac can be dangerous. NSAIDs like etodolac affect platelets and can thin your blood further. When paired with anticoagulants, this raises your risk of serious bleeding - in your stomach, brain, or elsewhere. The risk isn’t theoretical. In 2022, the U.S. FDA reported 1,100 emergency cases linked to NSAID-anticoagulant combinations, with nearly 20% requiring hospitalization.
Signs to watch for: black or tarry stools, unusual bruising, nosebleeds that won’t stop, or sudden headaches. If you’re on blood thinners and need pain relief, acetaminophen is usually the safer choice. But even then, check with your pharmacist - some formulations of acetaminophen contain hidden NSAIDs.
Etodolac and Corticosteroids
Corticosteroids like prednisone or dexamethasone are often prescribed for arthritis, asthma, or autoimmune conditions. When combined with etodolac, the risk of stomach ulcers and perforation skyrockets. Both drugs irritate the stomach lining, and together, they can cause damage so severe it requires emergency surgery.
A 2021 study in Arthritis & Rheumatology found that patients taking both an NSAID and a steroid had a 7 times higher risk of peptic ulcer complications than those taking only one. If you’re on a short-term steroid course, your doctor might suggest switching to a COX-2 inhibitor like celecoxib - which is less likely to cause ulcers - or adding a proton pump inhibitor (PPI) like omeprazole to protect your stomach.

Etodolac and SSRIs or SNRIs
Antidepressants like fluoxetine (Prozac), sertraline (Zoloft), or venlafaxine (Effexor) are common. But they also affect platelet function. When you add etodolac to the mix, your risk of bleeding increases - especially in the elderly or those with liver disease.
Studies show that people taking SSRIs with NSAIDs have a 2.5 times higher risk of upper gastrointestinal bleeding than those taking SSRIs alone. It’s not just stomach bleeding, either. There’s also a small but real risk of bleeding in the brain, especially after a fall or head injury. If you’re on an SSRI and need pain relief, ask your doctor about alternatives. Sometimes, physical therapy or heat therapy can reduce the need for NSAIDs altogether.
Etodolac and Lithium
If you’re taking lithium for bipolar disorder, etodolac can be especially risky. NSAIDs reduce how quickly your kidneys clear lithium from your body. That causes lithium levels to rise - sometimes dangerously high. Symptoms of lithium toxicity include tremors, confusion, slurred speech, nausea, and even seizures.
A 2023 case report in the Journal of Affective Disorders described a 68-year-old man who developed lithium toxicity after starting etodolac for knee pain. His lithium level jumped from 0.7 mmol/L to 1.8 mmol/L (the toxic range starts at 1.5). He had to be hospitalized. If you’re on lithium, your doctor should check your lithium levels within 3-5 days of starting etodolac. In many cases, they’ll avoid NSAIDs entirely and recommend acetaminophen or non-drug treatments.
Etodolac and Kidney Medications
Your kidneys handle both etodolac and many other drugs. If you’re taking medications that affect kidney function - like cyclosporine, tacrolimus, or certain antibiotics (aminoglycosides) - etodolac can make things worse. NSAIDs reduce blood flow to the kidneys, which can lead to acute kidney injury, especially in older adults or those with diabetes or heart failure.
Signs of kidney trouble: reduced urine output, swelling in ankles or feet, fatigue, or confusion. If you’re on these meds and your doctor prescribes etodolac, they should monitor your kidney function with a blood test before and after starting it. In some cases, they’ll avoid etodolac entirely and choose a safer alternative.

What to Do Instead
You don’t have to suffer through pain just because etodolac interacts with your other meds. Here are safer options:
- Acetaminophen (paracetamol) - Usually the best alternative. It doesn’t affect blood pressure, kidneys, or bleeding risk the way NSAIDs do. Stick to no more than 3,000 mg per day.
- Topical pain relievers - Gels or patches with diclofenac or menthol can help joint pain without affecting your whole body.
- Physical therapy or heat/cold therapy - For arthritis or muscle pain, these are proven to reduce reliance on pills.
- Low-dose capsaicin cream - Works well for osteoarthritis and has no systemic interactions.
Always talk to your pharmacist before starting any new medicine - even over-the-counter ones. They have access to drug interaction databases and can spot risks your doctor might miss.
When to Call Your Doctor
If you’re taking etodolac and notice any of these, call your doctor right away:
- Bloody or black stools
- Vomiting blood or material that looks like coffee grounds
- Sudden swelling in legs or ankles
- Shortness of breath or chest pain
- Unexplained bruising or bleeding
- Reduced urine output or dark urine
- Confusion, tremors, or slurred speech
These aren’t normal side effects - they’re warning signs. Don’t wait to see if they go away.
Final Tips
- Keep a list of all your meds - including supplements and herbal products - and update it every time something changes.
- Use one pharmacy for all your prescriptions. They’ll flag dangerous interactions automatically.
- Don’t assume natural supplements are safe. Fish oil, garlic, ginkgo, and ginger can also increase bleeding risk when mixed with etodolac.
- Ask your doctor: ‘Is there a non-NSAID option that won’t interfere with my other meds?’
Etodolac can be helpful - but only if you know what it’s doing with the rest of your body. The right combination of meds can keep you mobile and pain-free. The wrong one can land you in the hospital. Stay informed. Stay safe.
Can I take etodolac with Tylenol?
Yes, acetaminophen (Tylenol) is generally safe to take with etodolac. It works differently than NSAIDs and doesn’t increase bleeding or kidney risks. But don’t exceed 3,000 mg of acetaminophen per day, and avoid products that combine both drugs under one brand name. Always check labels.
Does etodolac raise blood pressure?
Yes, etodolac can raise blood pressure, especially in people who already have hypertension or are taking blood pressure medications. It can reduce the effectiveness of ACE inhibitors, ARBs, and diuretics. If you’re on these meds, monitor your blood pressure closely and report any upward trend to your doctor.
Is etodolac safe for people with kidney disease?
Etodolac is not recommended for people with moderate to severe kidney disease. It reduces blood flow to the kidneys and can cause acute kidney injury. If you have kidney issues, your doctor will likely avoid NSAIDs entirely and suggest alternatives like acetaminophen or physical therapy.
Can I drink alcohol while taking etodolac?
It’s best to avoid alcohol. Drinking while on etodolac increases your risk of stomach bleeding and liver damage. Even one or two drinks a day can be risky, especially if you’re older or have a history of ulcers. If you choose to drink, limit it to one drink occasionally and never on an empty stomach.
How long does it take for etodolac to leave the body?
Etodolac has a half-life of about 6 to 8 hours, meaning it takes roughly 2 days to fully clear from your system. But its effects on blood pressure, kidneys, and platelets can linger longer. If you’re switching to another medication or preparing for surgery, your doctor may ask you to stop etodolac 5 to 7 days in advance.
What to Do Next
If you’re currently taking etodolac and other medications, don’t stop or change anything on your own. Instead, schedule a medication review with your pharmacist or doctor. Bring your full list - pills, patches, supplements, even herbal teas. Many people don’t realize that St. John’s wort or turmeric can interact with etodolac too.
Ask: ‘Is there a safer way to manage my pain without risking interactions?’ Often, the answer isn’t another drug - it’s a change in lifestyle, physical therapy, or a different class of pain reliever. You don’t have to choose between pain and safety. There’s almost always a better path.





Christopher K
18 November, 2025 . 18:24 PM
Oh wow, another ‘read the fine print’ lecture from Big Pharma’s PR team. Next they’ll tell us not to breathe oxygen while taking aspirin. I’ve been popping etodolac with my blood pressure meds for 5 years and I’m still standing - unlike my neighbor who died from ‘natural supplements.’
harenee hanapi
20 November, 2025 . 10:14 AM
OMG I KNEW IT. My aunt took etodolac and then her lithium went wild and she started crying at the grocery store and wouldn’t stop saying ‘the walls are singing.’ I told her it was the NSAID but nooo, she said ‘it’s just menopause.’ Now she’s on disability and I’m her caregiver. I’m not even mad, just… spiritually exhausted. 🥲
Christopher Robinson
20 November, 2025 . 16:14 PM
Great breakdown - seriously, this is the kind of info that saves lives. 🙌 I’m a pharmacist and I see this every day. People think ‘it’s just a painkiller’ and don’t realize it’s like throwing gasoline on a fire when combined with anticoagulants or lithium.
Pro tip: If you’re on 3+ meds, walk into your pharmacy and say ‘I need a med sync.’ They’ll map everything out for free. Also - yes, Tylenol is usually your BFF here. Just don’t go over 3k mg/day. Your liver will thank you. ❤️
James Ó Nuanáin
22 November, 2025 . 02:19 AM
While the content presented is undoubtedly accurate and clinically sound, I must express my profound concern regarding the casual tone adopted throughout. In the United Kingdom, we maintain a certain decorum when discussing pharmacological risk - particularly in matters concerning renal function and gastrointestinal haemorrhage. One might argue that the proliferation of such informal digital discourse undermines public trust in medical authority.
That said, the inclusion of evidence-based references and clear clinical indicators is commendable. I shall be sharing this with my GP practice. 🇬🇧
Nick Lesieur
22 November, 2025 . 03:32 AM
So let me get this straight - I can’t take ibuprofen, aspirin, fish oil, turmeric, or alcohol with etodolac… but I can drink 3 energy drinks and smoke 2 packs a day? 🤡
Also, ‘ask your pharmacist’ - yeah, right. Last time I did that, they handed me a coupon for Sudafed and asked if I was ‘trying to make meth.’
Angela Gutschwager
22 November, 2025 . 20:59 PM
This post is correct. Stop ignoring your meds. 🚨
Andy Feltus
23 November, 2025 . 20:40 PM
Here’s the real question: Why do we treat pain like a bug to be eradicated instead of a signal to be listened to?
Etodolac doesn’t fix arthritis. It just silences the alarm. Meanwhile, we’re told to avoid alcohol, NSAIDs, fish oil, and now even ginger tea.
But nobody asks: Why are we in so much pain in the first place? Is it the sitting? The stress? The processed food? The fact that we’ve outsourced movement to algorithms and convenience?
Maybe the real interaction isn’t between drugs - it’s between our bodies and the way we live.
Just saying. 🤔
seamus moginie
25 November, 2025 . 10:52 AM
While I appreciate the clinical rigor of this post, I must emphasize that the underlying assumption - that pharmaceutical intervention is the primary solution - remains dangerously unchallenged. The notion that one must simply swap etodolac for acetaminophen, or ‘try physical therapy,’ betrays a fundamental ignorance of systemic healthcare failure.
Let us not forget: in Ireland, where I reside, access to physiotherapy is often contingent upon private insurance or bureaucratic patience. Meanwhile, the cost of a single month’s supply of safe analgesics exceeds the weekly wage of a minimum-wage worker.
So yes - acetaminophen is ‘safer.’ But safety without accessibility is a luxury. And we are not all privileged enough to choose it.
Perhaps the real interaction is not between drugs - but between policy and pain.