What Exactly Is a Biosimilar?
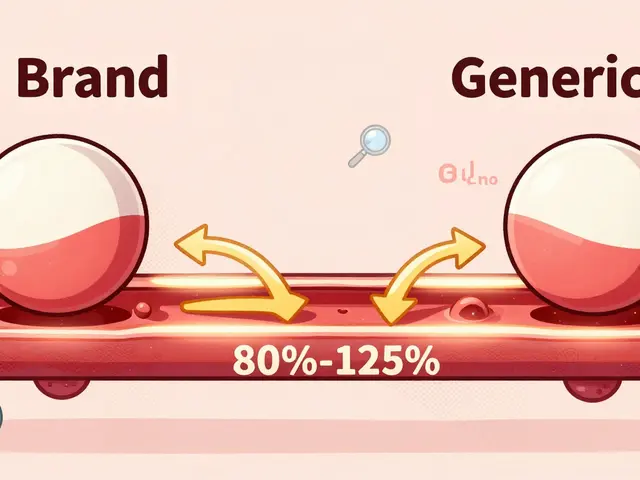
A biosimilar isn’t a generic drug. That’s the first thing to understand. Generics are exact chemical copies of small-molecule drugs like aspirin or metformin. Biosimilars, on the other hand, are highly similar versions of biologic drugs-complex proteins made from living cells. Think of them like identical twins raised in different homes: they look nearly the same, but subtle differences exist because of how they’re grown, purified, and handled.
These biologics treat serious conditions: cancer, rheumatoid arthritis, Crohn’s disease, diabetes, and osteoporosis. A single year of treatment for a reference biologic like adalimumab (Humira) can cost $50,000 to $100,000. Biosimilars aim to cut that price by 15% to 30%, but until recently, getting them approved in the U.S. was slow, expensive, and confusing.
The FDA’s Old Process Was a Bottleneck
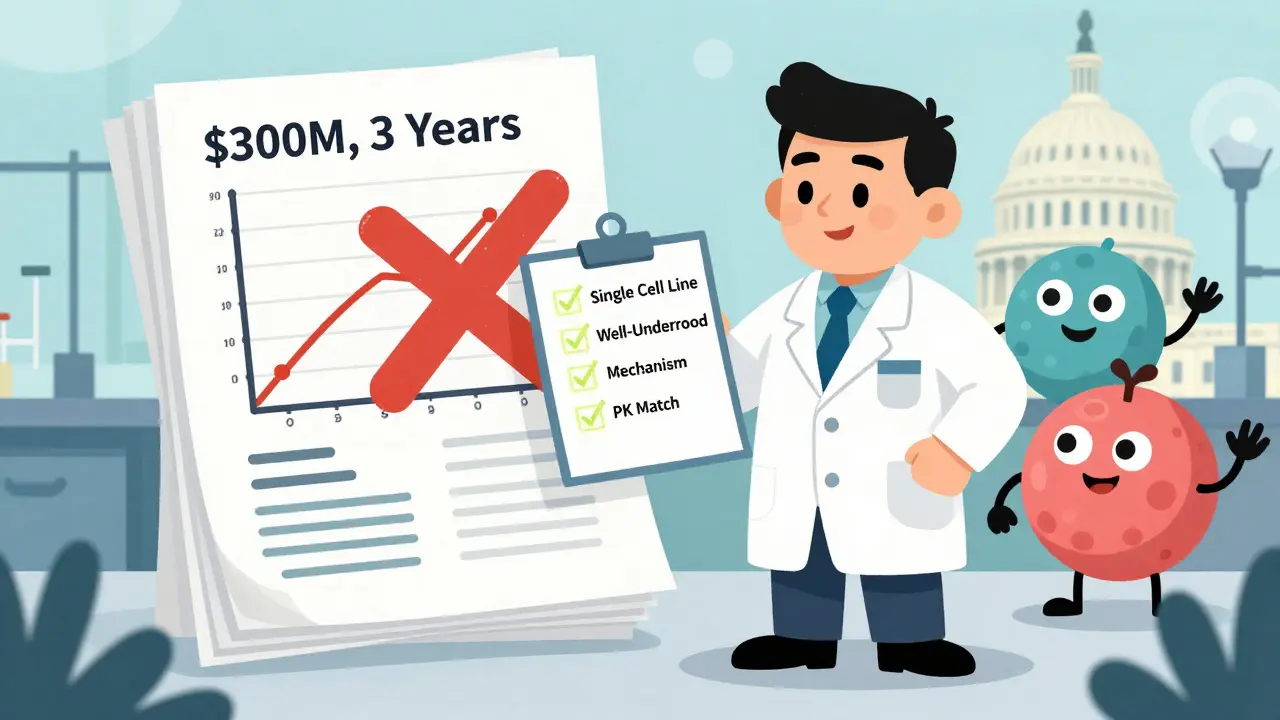
Before October 2025, the FDA required biosimilar sponsors to run full comparative clinical efficacy trials. These studies often took two to three years and cost between $100 million and $300 million. That’s why, despite 76 biosimilars being approved by the end of 2025, only 23% of eligible patients in the U.S. used them-compared to 67% in Europe.
Why the gap? The European Medicines Agency (EMA) had long accepted analytical and pharmacokinetic data as enough proof of similarity. The FDA, however, insisted on direct patient outcome comparisons-even when the science showed those differences were unlikely. Smaller companies couldn’t afford the trials. Big pharma held patents that delayed entry. The result? Patients waited years for cheaper options.
The Big Shift: FDA’s October 2025 Guidance
In October 2025, the FDA dropped its biggest update since the Biosimilar Pathway was created in 2010. The new draft guidance, titled Scientific Considerations in Demonstrating Biosimilarity, said: Stop running unnecessary clinical trials.
Now, if a biosimilar meets three criteria, you don’t need a full efficacy study:
- The drug is made from a single, well-characterized cell line and is highly purified.
- The link between its molecular structure and how it works in the body is well understood.
- A pharmacokinetic (PK) study in humans shows it behaves the same way in the bloodstream as the original.
That’s it. If those boxes are checked, analytical data from mass spectrometry, chromatography, and bioassays-testing over 200 quality attributes-is enough to prove biosimilarity. The FDA now says modern tools can predict clinical outcomes better than small, short-term patient trials.
Interchangeability: What It Means (and Doesn’t Mean)
Interchangeability is the holy grail. It lets pharmacists swap a biosimilar for the brand-name drug without asking the doctor. In the U.S., only a handful of biosimilars had this status before 2025.
The October 2025 guidance didn’t eliminate interchangeability-it changed how it’s assessed. The FDA no longer requires switching studies (where patients alternate between the reference and biosimilar). Commissioner Marty Makary said bluntly at a conference: “Every biosimilar should have the designation of interchangeable.”
But here’s the catch: the law still says interchangeability must be separately approved. So while the FDA is signaling it’s scientifically unnecessary, they’re still reviewing applications under the old legal framework. In October 2025, two denosumab biosimilars got interchangeability status-the first time multiple products for the same reference drug received it at once. That’s a sign the process is moving.
Who’s Winning and Who’s Struggling?
Big players like Sandoz, Pfizer, and Amgen still dominate, with 17, 12, and 10 approved biosimilars each. But the new rules are opening doors. Viatris and Biocon are gaining ground. The problem? Only 12 of the 76 approved biosimilars came from companies with fewer than 100 employees. Why? Because the analytical work is still expensive. You need labs capable of detecting tiny differences in protein folding or sugar attachments-tools most startups can’t afford.
That’s why the FDA’s Biosimilars User Fee Amendments (BsUFA III) matter. Since 2022, the agency has collected fees to fund faster reviews. Companies now get clear timelines: initial meetings within 7 days of filing, and decisions within 10 months for standard applications. The goal? Cut development time from 8-10 years to 5-7.

Real-World Impact: Savings and Skepticism
Mayo Clinic saved $18 million in one year by switching oncology patients to biosimilars. Hospital systems across the U.S. now include biosimilars in 89% of their formularies. That’s progress.
But patients? Only 32% have heard of biosimilars. A September 2025 Arthritis Foundation survey found 41% worried about safety. After talking to their doctors, 68% of those concerns disappeared. Reddit threads show mixed results: 63% report no difference in effectiveness, but 22% noticed more injection site reactions.
Doctors are cautious. Some fear subtle differences could build up over time in chronic conditions. Dr. Paul Baldrick warned in the Journal of Biological Sciences that long-term effects might still be missed. Meanwhile, PhRMA’s former chief scientist, Dr. Robert Popovian, argues that removing the interchangeability distinction without Congress changing the law creates confusion. If a pharmacist switches your drug without telling you, and you have a reaction, who’s liable?
What’s Next? The Road to 2030
The U.S. biosimilar market was worth $18.7 billion in 2024. By 2029, it’s projected to hit $62.3 billion. McKinsey forecasts biosimilars could capture 40-50% of the market by 2030-up from 23%. That’s $150 billion in annual savings.
But three hurdles remain:
- Patent litigation: The FTC says 68% of approved biosimilars face legal delays.
- State laws: 34 states still restrict pharmacist substitution, even though the FDA says interchangeability should be automatic.
- Complex molecules: Antibody-drug conjugates and other advanced biologics are harder to replicate. The new guidance doesn’t fully solve that yet.
The final version of the FDA’s 2025 guidance is expected in June 2026. If it sticks, we’ll see 15-20 new biosimilars approved each year instead of 8-10. That means more options, lower prices, and faster access.
Getting Started: What Developers Need to Know
If you’re a company trying to bring a biosimilar to market:
- Start early with an FDA pre-submission meeting. Use the Biosimilars Community Resource Center-it had over 12,000 visitors in October 2025.
- Invest in analytical tech. You need mass spectrometry, capillary electrophoresis, and functional bioassays.
- Don’t assume you need a clinical trial. Use the new guidance to argue against it.
- Plan for interchangeability. Even if you don’t ask for it now, build your data so you can apply later.
It’s still hard. But it’s easier than it was. And for patients waiting years for affordable treatment, that matters.


Murarikar Satishwar
3 February, 2026 . 06:34 AM
This is huge. The FDA finally getting real about biosimilars. No more wasting millions on redundant trials when we have mass spec and PK data that can predict outcomes better than a 200-patient study. This is how science should work.
India’s pharma sector is going to crush this. Companies like Biocon and Dr. Reddy’s are already building the analytical infrastructure. We’re not waiting for permission-we’re building the future.
Dan Pearson
4 February, 2026 . 04:08 AM
Oh wow, the FDA finally caught up to Europe? Took ‘em 15 years. Guess when you’re backed by Big Pharma lobbyists, you don’t rush to save people money. Meanwhile, Europe’s been saving billions and patients are getting treated. U.S. healthcare: still 10 years behind and proud of it.
clarissa sulio
5 February, 2026 . 18:06 PM
I’ve been in this industry for 18 years. This guidance is the most significant shift since the BPCIA passed. The science is solid. The data is robust. The only thing holding us back now is lawyers and state pharmacy boards.
Solomon Ahonsi
6 February, 2026 . 20:40 PM
So… we’re just skipping the clinical trials now? Cool. I guess if your drug looks the same under a microscope and acts the same in a test tube, it’ll be fine when someone’s got stage IV cancer on it. Sure. Why not.
George Firican
7 February, 2026 . 10:33 AM
There’s a philosophical layer here that’s being ignored. We’re not just talking about drug approval-we’re talking about trust. The human body isn’t a machine with interchangeable parts. Even if two proteins are 99.9% identical, the 0.1% difference might be the one that triggers an immune response in a subset of patients. Science can quantify similarity, but it can’t yet quantify the soul of a biological system. We’re optimizing for cost, not for complexity. And that’s dangerous.
Let’s not mistake efficiency for wisdom.
Vatsal Srivastava
8 February, 2026 . 10:23 AM
Biosimilars are just generics with a fancy name and a 10x price tag. The whole thing’s a scam. If it’s identical, why isn’t it cheaper? If it’s not identical, why are we calling it similar?
Brittany Marioni
10 February, 2026 . 08:57 AM
I’m so proud of the FDA for finally listening to the science! This is exactly what patient-centered care looks like! We need to make sure every patient, no matter their zip code, has access to these life-saving treatments! Let’s push for federal legislation to override state restrictions on interchangeability! And let’s fund public education campaigns so people aren’t scared of biosimilars! We can do this together!
Hannah Gliane
10 February, 2026 . 21:43 PM
So now pharmacists can swap your $100k drug for a $70k version without telling you? 😏 Good luck explaining to your dying uncle why his ‘Humira’ suddenly gave him a rash. Who’s gonna pay when the lawsuit happens? 🤔 #BigPharmaWin #FDAJustLiedToYou
Bob Hynes
11 February, 2026 . 01:53 AM
yo so like the FDA just said you don’t need clinical trials anymore? that’s wild. i mean, i get it, science is cool and all, but like… what if someone’s body just… reacts weird? like, i’ve had a friend who got sick from a ‘generic’ painkiller and it was just… different? you know? maybe we should just… keep testing? 🤷♂️
Nick Flake
11 February, 2026 . 03:07 AM
This is the moment we’ve been waiting for. The convergence of science, policy, and compassion. When we stop treating medicine like a corporate chess game and start treating it like a human right-this is what happens. Biosimilars aren’t just cheaper drugs. They’re dignity. They’re access. They’re hope for the 41% of patients who thought they’d never afford treatment. This isn’t policy. This is justice.
Let’s not celebrate with tweets. Let’s celebrate with action.
Akhona Myeki
11 February, 2026 . 11:39 AM
The FDA’s decision is a textbook example of regulatory capture disguised as innovation. In South Africa, we have no access to biosimilars because of intellectual property barriers. Meanwhile, the U.S. is streamlining approval for domestic manufacturers while maintaining trade protections that prevent low-income countries from producing their own. This is not progress. This is extraction.
Chinmoy Kumar
11 February, 2026 . 20:01 PM
this is so cool!! i just read about this and im like wow finally!! i hope more people know about this!! i have a cousin with ra and she pays like 2k a month for her med!! if this saves her even 500 a month its a win!! 🙏
Brett MacDonald
13 February, 2026 . 09:46 AM
The real question isn’t whether biosimilars work. It’s whether we’ve created a system where the only metric that matters is cost reduction. If we keep reducing medicine to a spreadsheet, we’ll eventually lose the human element entirely. Biosimilars might be cheaper. But are we becoming numb to the complexity of life?