Supplement Interaction Checker
Check Your Supplements Against Medications
This tool identifies dangerous interactions between common medications and supplements. Always consult your healthcare provider before combining medications.
Many people believe that if something is labeled "natural," it must be safer than a prescription drug. You see it on labels: "100% natural," "plant-based," "no chemicals." It sounds comforting. But here’s the truth: natural doesn’t mean safe. And when you mix herbal supplements with prescription meds, the risks aren’t theoretical-they’re happening every day, often without anyone noticing.
The Myth of "Natural = Safe"
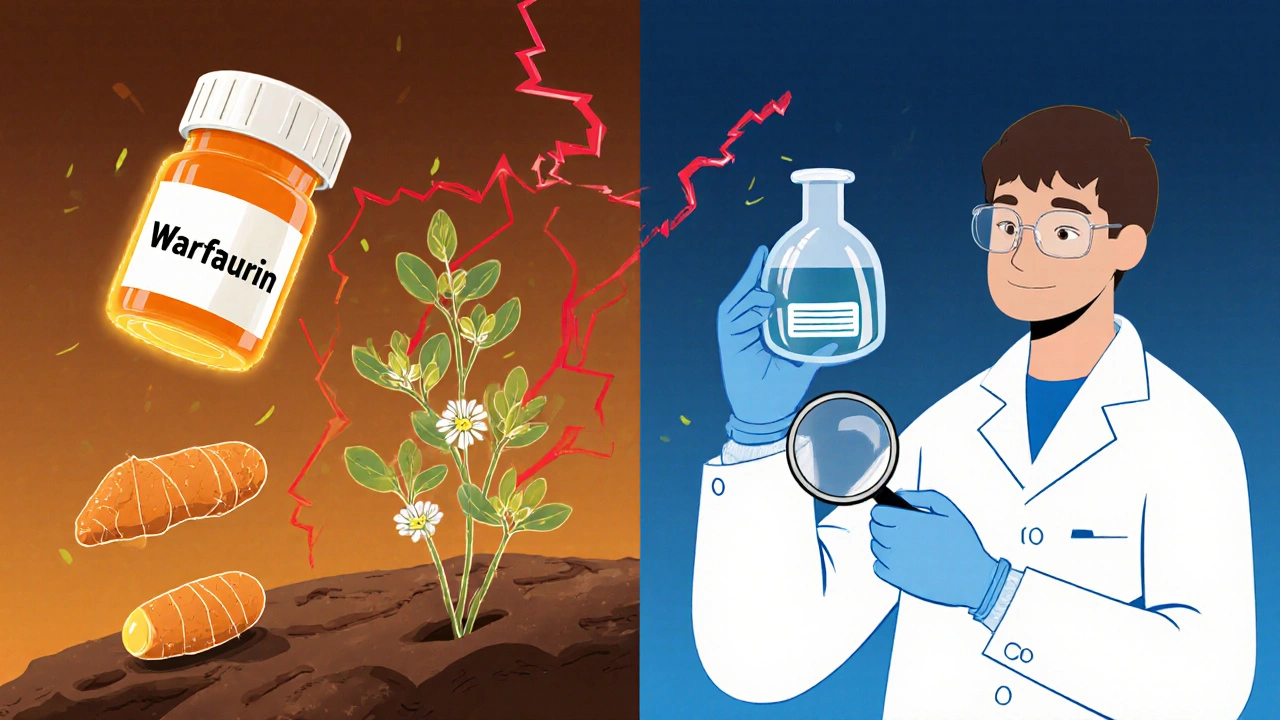
The idea that nature is inherently pure and better than science is deeply rooted in culture. It’s why people choose turmeric capsules over anti-inflammatories, or St. John’s wort instead of antidepressants. But nature doesn’t care if you feel better. It doesn’t know your medical history. And it doesn’t follow dosing guidelines. Take kava. It’s been used for centuries in the Pacific Islands for relaxation. But in the early 2000s, dozens of cases of severe liver damage were linked to kava supplements. Some people needed transplants. The FDA issued warnings. Kava was pulled from shelves in several countries. Yet it’s still sold today, often with no warning about liver risk. Or consider foxglove. The plant contains digitalis-a chemical used in heart medications like digoxin. Eat the leaves? You could die. But extract that same chemical, purify it, test it, and dose it precisely? That’s a life-saving drug. The difference isn’t nature vs. science. It’s control vs. chaos.How Regulators Treat Natural vs. Pharmaceutical Products
In the U.S., pharmaceuticals go through a gauntlet. Before a drug hits the shelf, it must pass multiple phases of clinical trials involving thousands of people. The manufacturer must prove it works, document every side effect, and show the factory where it’s made meets strict cleanliness and consistency standards. The FDA inspects those factories. They monitor reports of harm after the drug is sold. Herbal supplements? Not even close. Under the Dietary Supplement Health and Education Act (DSHEA) of 1994, supplements are classified as food-not medicine. That means companies don’t need to prove safety or effectiveness before selling. No clinical trials. No long-term safety data. No requirement to list all possible interactions. The FDA can only act after harm is reported-and even then, they’re underfunded and overwhelmed. A 2023 report showed the FDA issued just 35 warning letters to supplement makers that year. Meanwhile, thousands of products with unverified ingredients, heavy metal contamination, or hidden pharmaceuticals were still on Amazon and in health food stores.Where the Real Danger Lies: Interactions
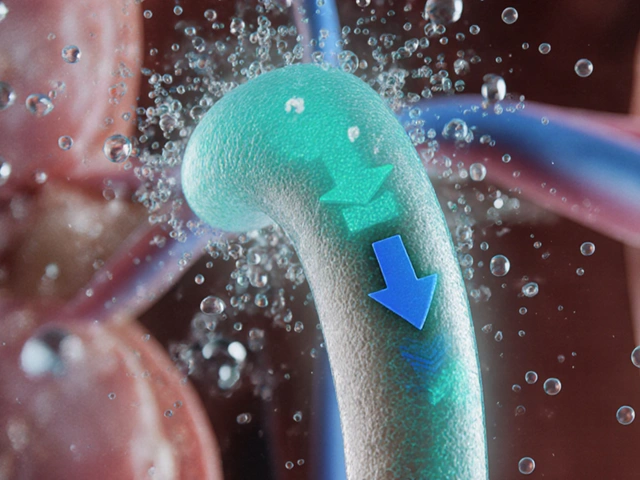
The biggest threat isn’t taking a supplement alone. It’s taking it with your other meds. St. John’s wort is one of the most dangerous offenders. It’s marketed for mild depression. But it can make birth control pills fail. It can reduce the effectiveness of blood thinners like warfarin. It can interfere with HIV meds, cancer drugs, and even antidepressants-sometimes triggering dangerous serotonin overload. Ginkgo biloba, often taken for memory, can thin your blood. If you’re on aspirin or clopidogrel, that’s a recipe for bleeding. A 2022 study found that over 40% of older adults taking ginkgo were also on blood thinners-and most didn’t tell their doctors. Even something as simple as vitamin K can mess with warfarin. Or grapefruit juice, which blocks enzymes that break down dozens of common drugs, causing toxic buildup. That’s not "natural"-that’s pharmacology. And it’s not optional. It’s life-threatening.
Numbers Don’t Lie-But They’re Misunderstood
You’ve probably heard: "100,000 people die each year from prescription drugs, but only a handful from herbs." That sounds reassuring. But it’s misleading. First, prescription drugs are used by millions daily, under medical supervision. Supplements? Often taken by people who don’t know what’s in them, or why. Second, adverse events from supplements are massively underreported. Most people don’t connect their stomach ache or dizziness to a new turmeric pill. Doctors rarely ask about supplements. The FDA’s MedWatch system recorded just 1,200 supplement-related reports in 2022-compared to 120,000 for prescription drugs. But experts agree that’s a fraction of the real number. A 2022 Consumer Reports survey found 68% of supplement users thought the FDA tests them for safety before sale. That’s false. The FDA doesn’t test supplements before they’re sold. They test them after someone gets hurt.What You’re Not Being Told About "Natural" Products
There’s no legal definition of "natural" in supplements. That means a product labeled "natural" could contain:- Contaminated herbs grown near highways (heavy metals)
- Fillers like talc or magnesium stearate
- Hidden pharmaceuticals-like sildenafil (Viagra) in "male enhancement" supplements
- Exactly the same active ingredient as a prescription drug, but without dosing control
Who’s at Highest Risk?
You might think this only affects older people or those on many meds. But it’s not that simple.- Seniors taking 5+ prescriptions are most vulnerable. They’re also the most likely to use supplements for "joint pain" or "memory support."
- People with chronic conditions-diabetes, heart disease, cancer-are at risk because their meds are tightly balanced.
- Women on birth control or hormone therapy can have their pills rendered useless by St. John’s wort or black cohosh.
- Even healthy people aren’t safe. A 20-year-old taking echinacea for a cold might unknowingly interfere with an upcoming surgery.
How to Protect Yourself
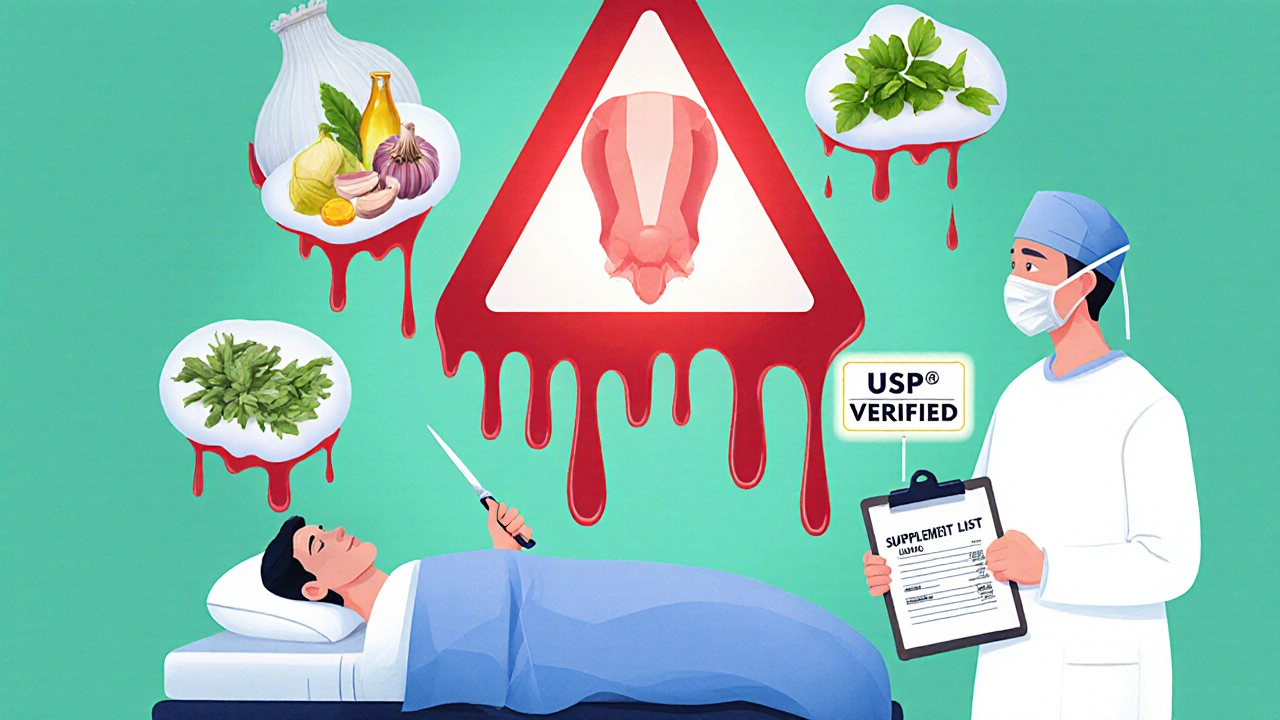
If you take supplements-or are thinking about it-here’s what to do:- Always tell your doctor and pharmacist-every single supplement, herb, vitamin, or tea you take. Even if you think it’s "just a little."
- Don’t trust labels. Look for third-party verification seals like USP Verified, NSF Certified, or ConsumerLab Approved. Only about 15% of supplement brands have these.
- Check interactions. Use the NIH’s Office of Dietary Supplements website. Type in your supplement and your medication. No guesswork.
- Stop before surgery. Most surgeons require you to stop all supplements two weeks before any procedure. Blood thinners like ginkgo, garlic, or fish oil can cause dangerous bleeding.
- Be skeptical of "miracle cures". If it claims to cure cancer, reverse aging, or replace your prescription, it’s likely fake or dangerous.
The Bigger Picture: Why This Keeps Happening
The supplement industry is worth $50 billion in the U.S. alone. That’s money chasing a belief: that nature is better. Companies don’t have to prove their products work. They just have to make them look good. Meanwhile, pharmaceutical companies spend $100 billion a year on R&D, face years of testing, and still get blamed for side effects. The system is unbalanced. And consumers are caught in the middle. But the science is clear: safety isn’t about whether something is natural or synthetic. It’s about quality, dosage, and awareness. A purified compound from a lab can save your life. A poorly made herbal extract can kill you.What’s Changing?
There’s hope. The Dietary Supplement Listing Act of 2023 is moving through Congress. It would require supplement makers to register their products with the FDA and list ingredients clearly. It’s not perfect-but it’s a step toward accountability. Some companies are already responding. Brands with USP Verified labels are growing. Independent labs are testing products for contaminants. Consumers are starting to ask: "Is this tested?" and "Can you show me the report?" The future of supplements won’t be about "natural vs. pharmaceutical." It’ll be about trustworthy vs. unverified. And that’s a shift we all need to push for.Are natural supplements regulated like prescription drugs?
No. Prescription drugs must pass rigorous clinical trials and FDA approval before sale. Supplements are classified as food under DSHEA, meaning they don’t need safety or effectiveness proof before hitting the market. The FDA only steps in after harm is reported.
Can herbal supplements really interfere with my medications?
Yes. St. John’s wort can reduce the effectiveness of birth control, antidepressants, and blood thinners. Ginkgo biloba can increase bleeding risk when taken with aspirin or warfarin. Even common herbs like garlic, ginger, or echinacea can interact with surgery meds or immune drugs. Always check interactions before taking anything new.
Why do so many people think natural means safe?
It’s a psychological bias. People associate "natural" with purity, tradition, and safety-often because of marketing. But nature includes poison ivy, arsenic, and deadly mushrooms. Safety depends on dosage, purity, and how it interacts with your body-not whether it came from a plant or a lab.
What should I look for on a supplement label?
Look for third-party verification seals: USP Verified, NSF Certified, or ConsumerLab Approved. These mean the product was independently tested for ingredients, purity, and contamination. Avoid products with vague claims like "all-natural" or "proprietary blend"-they hide what’s actually inside.
Is it safe to take supplements during pregnancy?
Many are not. While some prenatal vitamins are safe and recommended, other supplements like black cohosh, dong quai, or high-dose vitamin A can harm fetal development. Always consult your OB-GYN before taking anything-even if it’s labeled "natural."
Can I trust supplements sold on Amazon or in health food stores?
Not without verification. Many supplements sold online contain contaminants, fillers, or hidden drugs. A 2021 study found nearly a third of herbal supplements didn’t contain the herb listed on the label. Stick to brands with USP or NSF certification, and avoid anything that sounds too good to be true.
Do I really need to tell my doctor about my supplements?
Yes. A 2022 study showed 70% of patients don’t disclose supplement use to their doctors-even though it can affect diagnosis, treatment, and drug safety. Your doctor needs the full picture to keep you safe.


Scott Macfadyen
18 November, 2025 . 01:29 AM
Been taking turmeric for my knees for years. Never thought to check if it messed with my blood pressure med. Guess I’m lucky so far. But after reading this? I’m calling my pharmacist tomorrow. No more guessing games.
Alex Czartoryski
19 November, 2025 . 10:34 AM
Oh please. So now we’re supposed to trust Big Pharma over grandma’s herbal remedies? Next you’ll say aspirin is safer than willow bark. Wake up. The system’s rigged. Supplements are the only thing keeping regular folks from getting bankrupted by co-pays.
Andrea Johnston
19 November, 2025 . 11:44 AM
Let me guess - you’re the type who thinks ‘natural’ means ‘no side effects’ because it’s on a label with a picture of a leaf. Newsflash: arsenic is natural. Hemlock is natural. So is the mold on your fridge. Your body doesn’t care if it came from a lab or a forest. It only cares if it kills you. Stop romanticizing ignorance.
Denise Cauchon
19 November, 2025 . 19:54 PM
Canada’s got it right. We don’t let just anyone slap ‘natural’ on a bottle and sell it like medicine. But here in the States? It’s the Wild West. I’m not surprised you’ve got more people dying from supplements than from bad wine.
Gizela Cardoso
20 November, 2025 . 00:48 AM
My mom takes ginkgo for memory and warfarin for AFib. She didn’t even know they could interact. I printed out the NIH interaction checker and showed her. She cried. Then she threw out half her supplement drawer. We need more of this info - not less.
Duncan Prowel
20 November, 2025 . 05:19 AM
The regulatory asymmetry between pharmaceuticals and dietary supplements is not merely a policy failure - it is a systemic epistemic vulnerability. The burden of proof is inverted, and the consumer, lacking access to transparent, standardized data, becomes the de facto experimental subject. This is not libertarianism; it is negligence dressed as choice.
Jonathan Gabriel
20 November, 2025 . 14:20 PM
lol i just googled ‘st johns wort + my med’ and it said ‘can cause serotonin syndrome’ so i stopped taking it. but like… why do i have to google this? shouldn’t the bottle say ‘DANGER: WILL MAKE YOUR ANTIDEPRESSANT USELESS’? they don’t. because they’re not forced to. and that’s f***ing insane.
Victoria Malloy
20 November, 2025 . 14:32 PM
Thank you for writing this. I’ve been too scared to say anything because everyone says ‘natural is better’ - but I’ve seen too many people get sick from supplements. I’m telling my sister to stop taking that ‘immune booster’ she got from her yoga teacher. It’s not about being anti-nature. It’s about being pro-safety.
Chloe Sevigny
20 November, 2025 . 15:26 PM
It’s not the supplements themselves that are the problem - it’s the epistemological collapse of public discourse. We’ve replaced evidence-based reasoning with aesthetic tribalism: ‘green label = good’, ‘white pill = evil’. The irony? The very people who reject pharmaceuticals as ‘corporate poison’ are the same ones who buy $40 bottles of ‘detox tea’ with no clinical data - and then blame the FDA for not regulating it. The hypocrisy is breathtaking.
Bruce Bain
20 November, 2025 . 20:46 PM
My cousin took a ‘natural’ sleep aid and ended up in the ER. Turns out it had melatonin and benadryl - both legal, but not together, and not at that dose. No label said that. He’s fine now, but we’re all talking about it. Just… please, ask your doctor. Even if it’s ‘just a pill’.