Hypoglycemia Risk Calculator
Personalized Hypoglycemia Risk Assessment
Answer a few questions to estimate your risk of low blood sugar when taking diabetes medications.
Low Risk: Hypoglycemia is unlikely at recommended doses.
Medium Risk: Monitor blood sugar regularly; adjust diet/exercise.
High Risk: Consider alternative medications; consult your doctor.
Risk Comparison
| Medication | Relative Risk | Key Considerations |
|---|---|---|
| Micronase (Glyburide) | High | Higher hypoglycemia risk, especially in elderly patients |
| Metformin | Low | Minimal risk of hypoglycemia; first-line recommendation |
| Glipizide | Moderate | Lower risk than glyburide but still requires monitoring |
| Sitagliptin | Very Low | No hypoglycemia when used alone; weight neutral |
Quick Takeaways
- Micronase (glyburide) is a second‑generation sulfonylurea that lowers blood sugar by boosting insulin release.
- It works fast but carries a higher risk of hypoglycemia than metformin or newer agents.
- Glipizide and glimepiride are similar sulfonylureas with slightly lower hypoglycemia risk.
- Metformin, a biguanide, is usually first‑line because it improves insulin sensitivity with minimal weight gain.
- Newer classes like DPP‑4 inhibitors (e.g., sitagliptin) and SGLT2 inhibitors (e.g., empagliflozin) offer lower hypoglycemia risk but at higher cost.
When it comes to managing type 2 diabetes, picking the right pill can feel like a gamble. Micronase often shows up on prescriptions because it’s inexpensive and effective at dropping glucose levels, yet many patients wonder if there’s a safer or more convenient option. This guide breaks down Micronase (glyburide) side‑by‑side with the most common alternatives, so you can see exactly how they differ in action, side effects, cost, and who benefits most.
What is Micronase (Glyburide)?
When treating type 2 diabetes, Micronase is a brand name for glyburide, a second‑generation sulfonylurea that stimulates insulin release from pancreatic β‑cells. Glyburide belongs to the sulfonylurea class, which has been on the market since the 1960s. It is typically prescribed when diet, exercise, and metformin alone cannot keep HbA1c within target range.
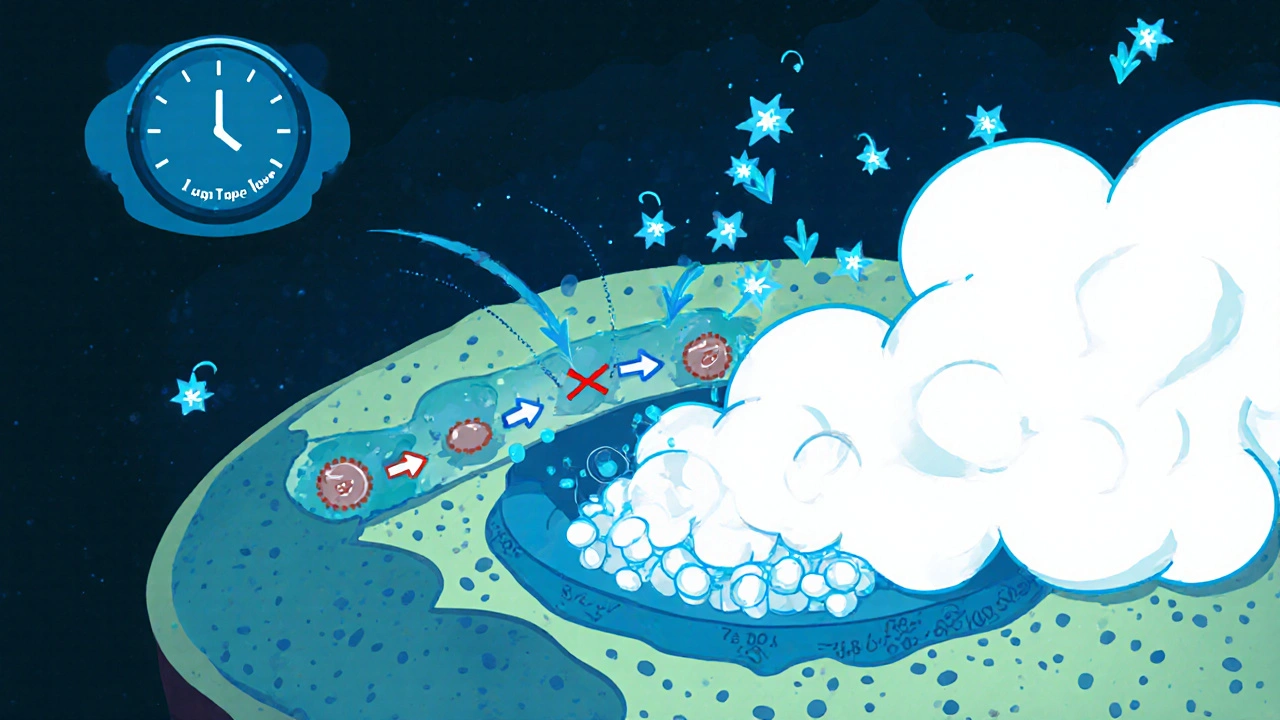
How Micronase Works
Glyburide binds to the sulfonylurea receptor (SUR1) on the pancreatic beta cell surface. This binding closes ATP‑sensitive potassium channels, leading to cell depolarization and calcium influx. The calcium surge triggers insulin granule exocytosis, flooding the bloodstream with insulin. The result is a rapid drop in post‑prandial glucose, usually within 30-60 minutes of taking the dose.
Key Attributes of Micronase
- Typical dose: 2.5 mg to 10 mg once daily, taken with breakfast.
- Onset of action: 30-60 minutes.
- Peak effect: 4-6 hours.
- Half‑life: 10-12 hours, allowing once‑daily dosing for most patients.
- Common side effects: hypoglycemia, weight gain, nausea, and occasional skin rash.
- Contraindications: severe liver disease, renal failure (eGFR < 30 mL/min), and pregnancy.
Alternatives to Micronase
Below are the most frequently considered alternatives, grouped by drug class.
- Glipizide - another second‑generation sulfonylurea with a slightly shorter half‑life.
- Glimepiride - third‑generation sulfonylurea, often praised for lower hypoglycemia risk.
- Metformin - biguanide that improves insulin sensitivity; first‑line in most guidelines.
- Sitagliptin - DPP‑4 inhibitor that increases endogenous GLP‑1, providing modest glucose control with minimal weight impact.
- Empagliflozin - SGLT2 inhibitor that forces glucose loss via urine, also offers cardiovascular benefits.
Comparison Table
| Medication | Class | Typical Dose | Onset | Hypoglycemia Risk | Weight Effect | Cost (AU$ per month) |
|---|---|---|---|---|---|---|
| Micronase (Glyburide) | Sulfonylurea | 2.5‑10 mg daily | 30‑60 min | High | Gain 1‑3 kg | ≈30 |
| Glipizide | Sulfonylurea | 2.5‑10 mg daily | 30‑60 min | Medium | Gain 0‑2 kg | ≈35 |
| Glimepiride | Sulfonylurea | 1‑4 mg daily | 30‑60 min | Medium‑Low | Gain 0‑2 kg | ≈40 |
| Metformin | Biguanide | 500‑2000 mg BID | 2‑3 hrs | Low | Neutral or loss | ≈20 |
| Sitagliptin | DPP‑4 inhibitor | 100 mg daily | 1‑2 hrs | Very Low | Neutral | ≈120 |
| Empagliflozin | SGLT2 inhibitor | 10‑25 mg daily | 1‑2 hrs | Very Low | Loss 1‑3 kg | ≈150 |
Pros and Cons of Micronase Compared to Each Alternative
Micronase vs Glipizide
Both are sulfonylureas, but glipizide’s shorter half‑life (≈4 hours) means a lower chance of overnight hypoglycemia. If you struggle with early‑morning lows, glipizide might feel safer. However, the glucose‑lowering power is almost identical, so the choice often hinges on side‑effect profile and price.
Micronase vs Glimepiride
Glimepiride is marketed as having the lowest hypoglycemia risk among sulfonylureas. It also has a modest weight‑neutral effect. The trade‑off is a slightly higher price and the need for careful dose titration, especially in elderly patients.
Micronase vs Metformin
Metformin works on a completely different pathway-improving insulin sensitivity in the liver and muscle. It rarely causes hypoglycemia and can even promote modest weight loss. The downside: gastrointestinal upset is common, and it’s contraindicated in severe renal impairment. For many clinicians, metformin stays first‑line, while Glyburide (Micronase) is a backup when metformin alone isn’t enough.
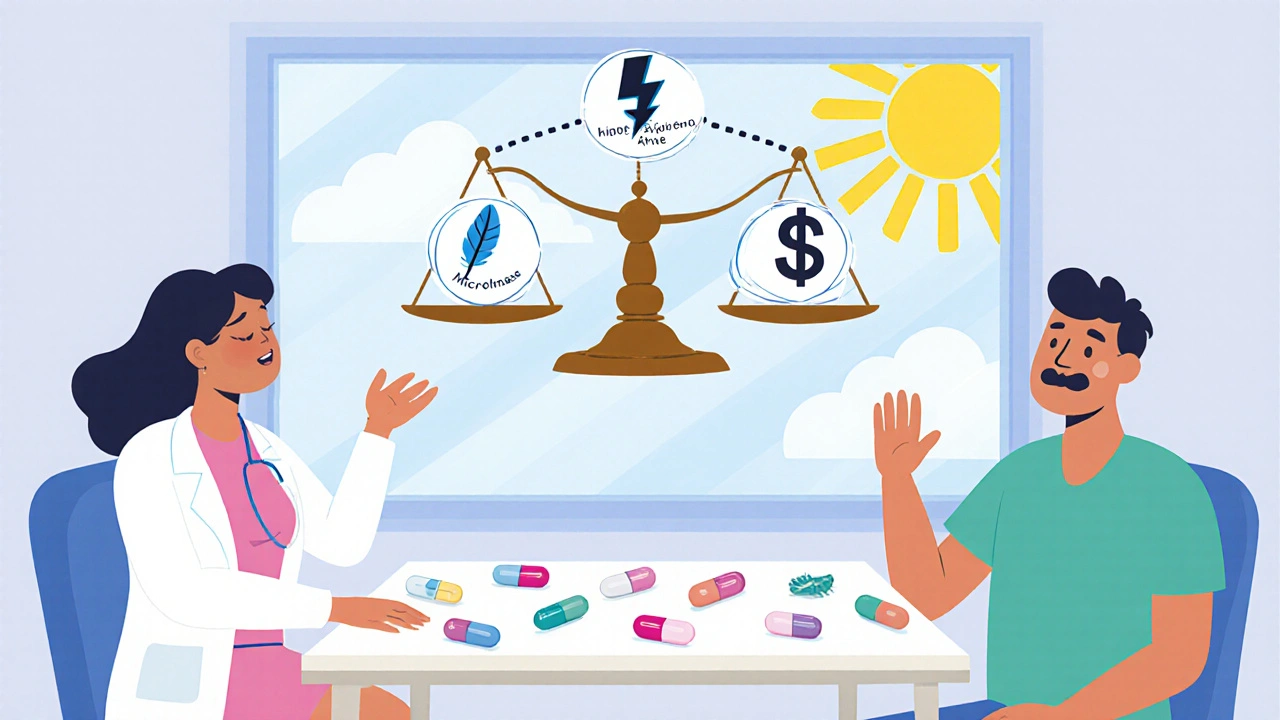
Micronase vs Sitagliptin (DPP‑4 inhibitor)
Sitagliptin adds only about 0.5‑0.8 % HbA1c reduction on top of existing therapy, but its biggest selling point is the negligible hypoglycemia risk. It’s also weight‑neutral. The catch? It’s more than three times as expensive as Micronase in Australia, which can be a barrier for patients without private insurance.
Micronase vs Empagliflozin (SGLT2 inhibitor)
Empagliflozin not only lowers glucose but also reduces cardiovascular events and slows kidney disease progression-a big plus for high‑risk patients. It also tends to cause weight loss. However, it can raise the risk of urinary tract infections and is pricey. Micronase does not offer these extra organ‑protective benefits.
How to Choose the Right Medication
Decision‑making should weigh four main factors:
- Risk of hypoglycemia: If you have a history of lows, steer toward metformin, sitagliptin, or empagliflozin.
- Weight considerations: Patients trying to lose weight usually avoid sulfonylureas and favor metformin or SGLT2 inhibitors.
- Cost & insurance coverage: Micronase and other sulfonylureas are the cheapest options; newer agents may require government or private subsidy.
- Comorbidities: Cardiovascular disease or chronic kidney disease makes empagliflozin attractive; liver disease limits sulfonylurea use.
Always discuss these points with a qualified healthcare professional. Dosage adjustments, periodic lab monitoring, and lifestyle changes are essential regardless of which drug you end up using.
Common Questions (FAQ)
Can I switch from Micronase to Metformin?
Yes, most doctors will transition patients by gradually tapering the sulfonylurea while introducing metformin. This helps avoid sudden glucose spikes and reduces hypoglycemia risk during the switch.
Why does Micronase cause weight gain?
Sulfonylureas increase insulin levels, and insulin is an anabolic hormone that promotes fat storage. The effect is modest compared with insulin therapy, but it’s noticeable over months.
Is Micronase safe for pregnant women?
No. Glyburide crosses the placenta and has been linked to neonatal hypoglycemia. Insulin or metformin are preferred during pregnancy.
How often should I monitor blood sugar while on Micronase?
At least once daily, preferably fasting. If you experience symptoms of low blood sugar, check more frequently until you know how the medication affects you.
Can I combine Micronase with a DPP‑4 inhibitor?
Yes, many clinicians add a DPP‑4 inhibitor when sulfonylurea alone isn’t enough. The combination provides extra glucose control with a relatively low added hypoglycemia risk, but watch for cost.
Next Steps & Troubleshooting
- Experiencing frequent lows? Talk to your doctor about dose reduction or switching to a lower‑risk agent like glimepiride or metformin.
- Gaining weight? Pair Micronase with lifestyle counseling, or consider an SGLT2 inhibitor if budget permits.
- Renal function declines? Micronase should be discontinued once eGFR drops below 30 mL/min; switch to metformin (if eGFR > 45) or an SGLT2 inhibitor approved for lower renal function.
- Cost is a barrier? Generic glyburide tablets are widely available and often covered by Australian Pharmaceutical Benefits Scheme (PBS). Ask your pharmacist about the cheapest option.
Choosing a diabetes medication isn’t a one‑size‑fits‑all decision. By understanding how Micronase stacks up against glipizide, glimepiride, metformin, sitagliptin, and empagliflozin, you can have a data‑driven conversation with your healthcare provider and land on the therapy that matches your health goals, budget, and lifestyle.






Megan Dicochea
25 October, 2025 . 19:43 PM
Micronase does its job quickly but you have to watch the lows. The price point is hard to beat for people on a tight budget. It’s also true that the weight gain can be frustrating over time. If you’re prone to hypoglycemia you might want to discuss alternatives with your clinician.
Jennie Smith
28 October, 2025 . 07:50 AM
Hey folks, diving into the nitty‑gritty of diabetes meds can feel like painting a rainbow on a cloudy day – vibrant and full of possibilities! Micronase shines for its rapid action, but the hypoglycemia shadow looms large. If you’re chasing a balance between cost and safety, think of metformin as the steady drumbeat and the newer SGLT2 crew as the electrifying solo. Keep the conversation flowing and remember you’re the artist of your own health canvas!
Anurag Ranjan
30 October, 2025 . 20:57 PM
Think of glyburide as a short‑acting insulin secretagogue. It lowers glucose fast but the hypoglycemia risk is real. Pair it with careful monitoring and a clear diet plan.
James Doyle
2 November, 2025 . 10:03 AM
The pharmacodynamic profile of glyburide epitomizes the quintessential sulfonylurea principle, engaging the ATP‑sensitive potassium channels with a potency that belies its age. From a mechanistic standpoint, the downstream calcium influx precipitates an exocytotic cascade that, while efficacious, inexorably raises the specter of iatrogenic hypoglycemia. Clinicians must therefore calibrate the dose–response curve with scrupulous vigilance, lest the therapeutic window narrow to a perilous brink. In comparative pharmaco‑economic analyses, Micronase consistently emerges as a cost‑effective contender, yet its marginal cost advantage does not absolve the practitioner from assessing patient‑specific risk stratifiers. The weight gain trajectory observed in longitudinal cohorts underscores the anabolic ramification of chronic hyperinsulinemia induced by sulfonylurea therapy. When juxtaposed with metformin's insulin‑sensitizing mechanism, the latter's favorable impact on hepatic gluconeogenesis renders it the preferred first‑line agent in most guideline algorithms. Nevertheless, the pragmatic reality of medication adherence in socioeconomically disadvantaged populations often necessitates the inclusion of generic glyburide as a bridge therapy. From a cardiovascular outcomes perspective, the data remain equivocal, with some meta‑analyses hinting at modest adverse signals, thereby compelling a nuanced risk‑benefit discourse. The renal clearance considerations impose additional constraints, particularly in patients with eGFR thresholds below thirty milliliters per minute, where glyburide accumulation becomes a toxic possibility. Furthermore, the drug's interaction profile with CYP2C9 polymorphisms can amplify plasma concentrations, demanding genotype‑guided dosing adjustments in precision medicine frameworks. The advent of DPP‑4 and SGLT2 inhibitors introduces therapeutic agents with a markedly attenuated hypoglycemia propensity, albeit at a premium price point that may be prohibitive for cash‑pay patients. In the context of polypharmacy, the additive effect of sulfonylureas with other glucose‑lowering agents mandates vigilant surveillance for synergistic hypoglycemic episodes. Patient education remains a cornerstone; a thorough understanding of symptomatology, such as diaphoresis and neuroglycopenic manifestations, can forestall emergent crises. Health systems should incorporate algorithmic decision support tools that flag high‑risk prescriptions, thereby optimizing clinical pathways. Ultimately, the selection of Micronase must be predicated upon an integrative assessment encompassing glycemic targets, comorbid conditions, and socioeconomic determinants. A judicious, individualized approach will harness the drug's efficacy while mitigating its inherent hazards.
Justin Scherer
4 November, 2025 . 23:10 PM
James makes solid points about risks, and I’d add that patient preference plays a big role too. If cost is the main driver, Micronase can still be a viable option with proper monitoring.
Cheyanne Moxley
7 November, 2025 . 12:17 PM
Honestly, if you’re still debating cheap pills over real solutions you’re missing the point. Stop sugar‑coating the hype and get on a modern regimen.
Kevin Stratton
10 November, 2025 . 01:23 AM
Cheyanne, I get the frustration but hype isn’t the enemy 😊 proper education and tailored therapy are.
Lionel du Plessis
12 November, 2025 . 14:30 PM
Cheap and works.
Andrae Powel
15 November, 2025 . 03:37 AM
Reading through this guide, it’s clear that each medication has its own niche. For anyone feeling overwhelmed, start by tracking your blood sugars and noting any patterns of lows. That data will give your doctor a solid foundation to tailor the therapy.
Leanne Henderson
17 November, 2025 . 16:43 PM
Absolutely, Andrae – your suggestions are spot‑on, and I’d emphasize that consistent logging, honest communication with your healthcare team, and a willingness to adjust lifestyle habits can make a huge difference, especially when navigating the trade‑offs between efficacy, cost, and side‑effects.
Greg Galivan
20 November, 2025 . 05:50 AM
Micronase is cheap but dont think its a free pass for anything. You still need to watch the lows or you’ll end up in the ER.
Edward Brown
22 November, 2025 . 18:57 PM
Sure Greg, but have you considered that the pharma giants push cheap sulfonylureas to keep us hooked on their next big profit machine? They hide the long‑term damage while marketing it as budget friendly.
ALBERT HENDERSHOT JR.
25 November, 2025 . 08:03 AM
Edward, while vigilance is important, the evidence still supports glyburide as a cost‑effective option when used responsibly 😊. A balanced view that weighs clinical data against individual circumstances will serve patients best.